Are you looking to exercise your sprained ankle without risking further damage? This guide provides the essential steps for exercising a sprained ankle to support a safe and effective recovery. Learn the precise movements and strategies that help restore strength and flexibility, starting with the most gentle exercises and advancing as your ankle heals. Begin your journey to recovery with confidence, backed by expert advice and structured progression.
Key Takeaways
- Ankle sprains range from minor ligament stretching to severe high-grade sprains; recovery strategies must be tailored to the specific type and severity of the sprain.
- Early recovery should employ the RICE method and gradually introduce weight bearing and movements while avoiding prolonged immobilization to prevent secondary damage.
- Rehabilitation involves gentle range of motion exercises followed by progressive strengthening, balance and proprioception workouts, and advanced functional training, with supportive gear to enhance stability and reduce reinjury risk.

Understanding Your Sprained Ankle
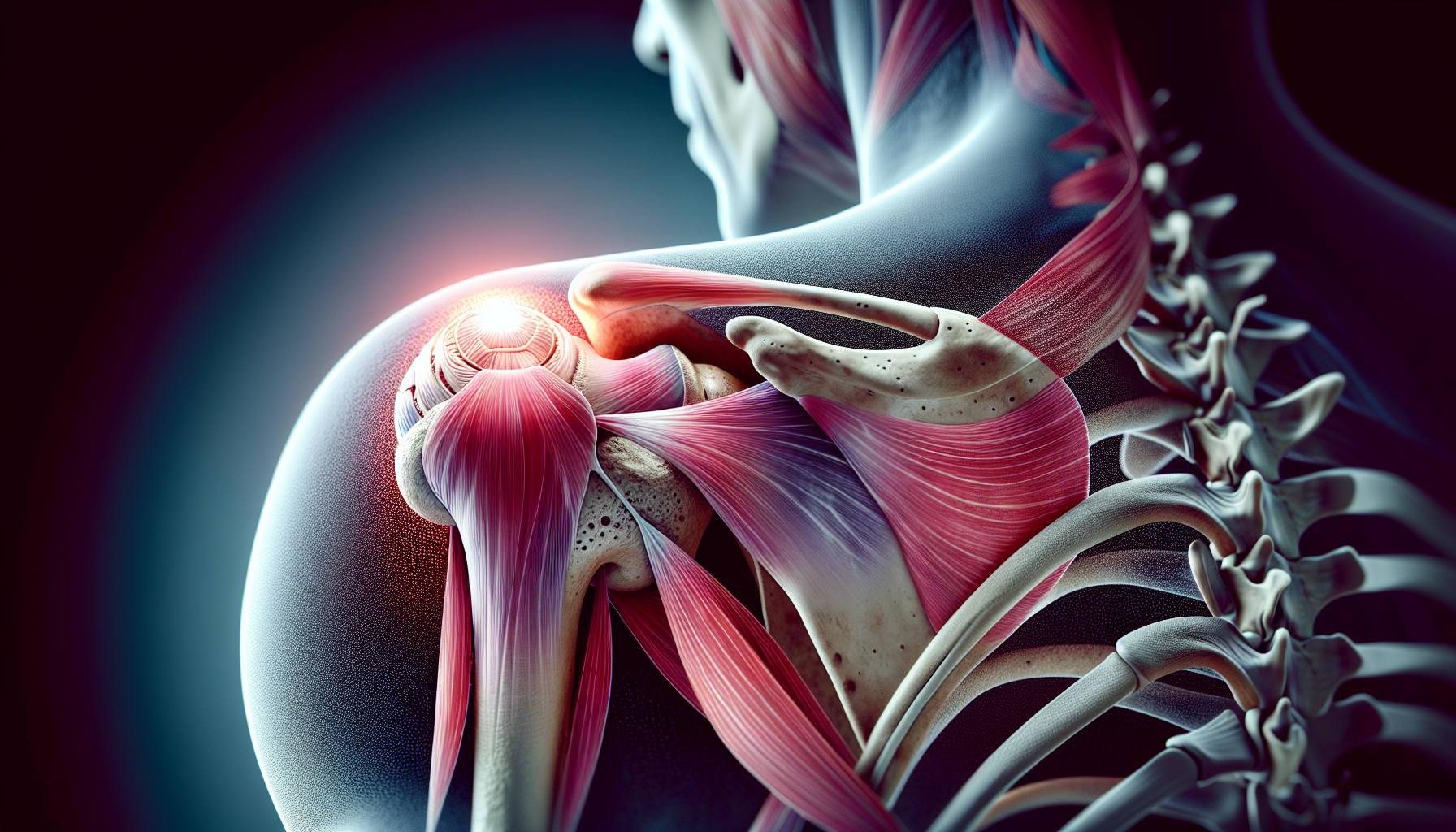
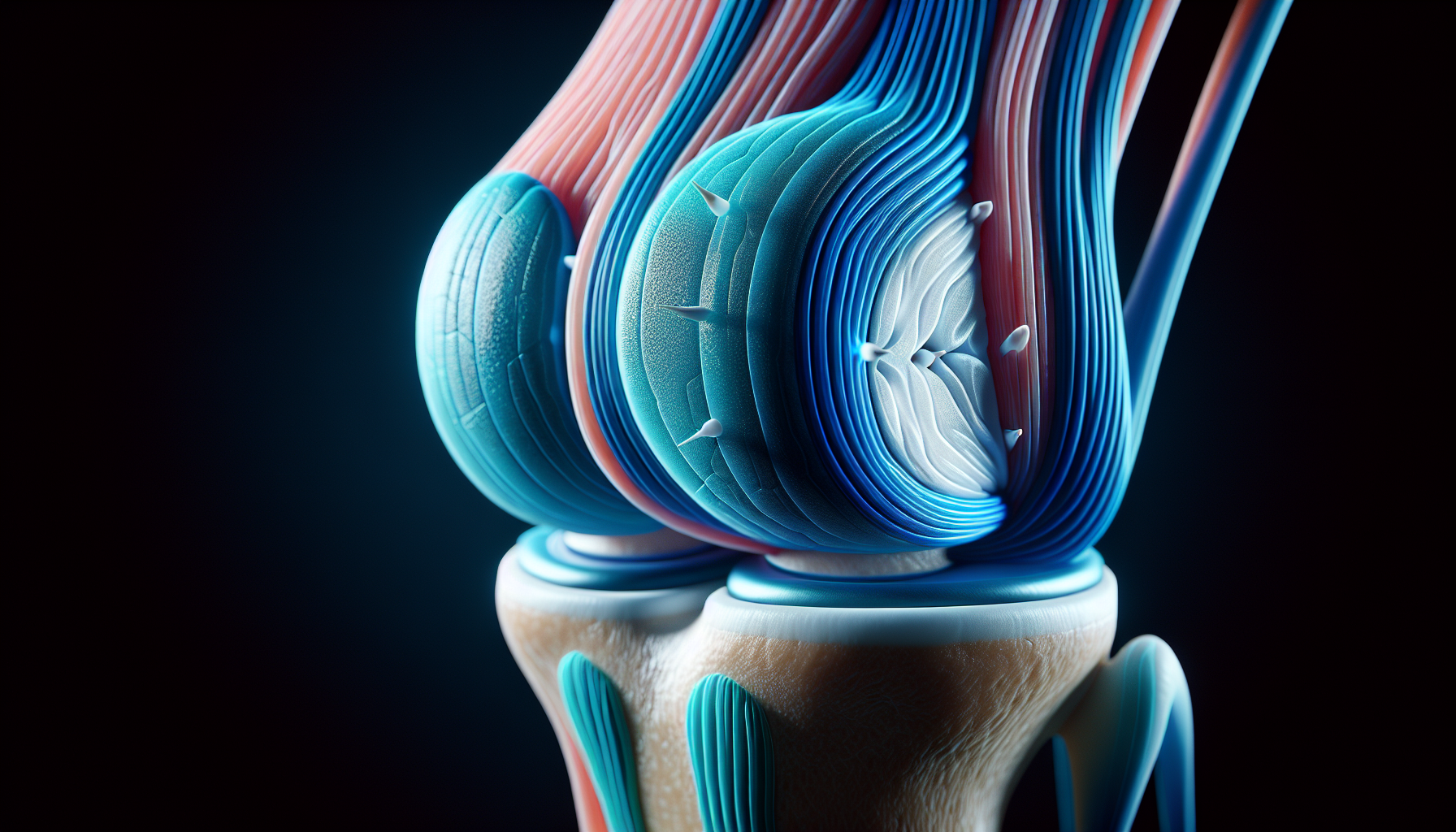
An ankle sprain, a common injury often linked to sports activities, involves damage to the ligaments that support the ankle joint. This complex joint is composed of three bones: the tibia, fibula, and talus. These bones are held together and supported by three main ligamentous systems: the lateral ligament complex, medial deltoid ligament, and syndesmotic ligaments. An injured leg, particularly an ankle sprain, requires proper care and treatment to ensure a full recovery.
Ankle sprains are often caused by the inversion of the foot, which puts stress on the lateral ligament complex, particularly the anterior talofibular ligament (ATFL). The medial deltoid ligament, the strongest of the ankle ligaments, is usually injured during eversion injuries. The type and severity of an ankle injury, or even an injured foot, can vary depending on the position of the foot and the type of rotational force applied.
Ankle sprain severities range from low-grade, involving ligament stretching or minor tears, to high-grade sprains that may include injury to the syndesmotic ligaments. Understanding the specifics of the injured ankle is crucial for determining an appropriate rehabilitation approach, especially in cases of an acute ankle sprain. Syndesmotic injuries, also referred to as ‘high ankle sprains’, are less common and typically affect competitive athletes.
Initial Steps to Exercise Post-Sprain
The initial steps post-sprain are crucial for effective recovery. The RICE method, which stands for Rest, Ice, Compression, and Elevation, is a recommended approach to reduce swelling and manage pain. Once immediate care has been addressed, rehabilitation should start promptly, focusing on reducing swelling, pain, and inflammation while protecting the joint from secondary damage due to excessive early exercises.
Gradual weight-bearing and comfortable movements, like supported walking for minor sprains, should be introduced within the first week, aligning with Plancher’s advice to foster healing. The common mistake of prolonged immobilization should be avoided by applying controlled stress to the injured area.
Protecting the ankle during the early stages is crucial, with later stages incorporating careful stress under supervision to aid the recovery process. Rehabilitation exercises should be tailored to the individual’s specific condition, following a doctor’s advice.
Gentle Range of Motion Exercises
Once the initial care phase has been navigated successfully, it’s time to begin gentle range of motion exercises, focusing on knee motion. To begin these exercises, support the leg while allowing the foot and ankle to hang freely, typically done by performing a knee motion sit and positioning the leg on another chair.
Engage in a series of exercises to promote a gentle range of motion in the sprained ankle. These exercises include:
- ‘Flex’
- ‘Extend’
- Inward and outward bends
- Ankle circles
- Foot alphabet exercises
Perform each exercise by holding each position for 10 to 15 seconds and repeating the movements 10 times, twice a day.
These gentle range of motion exercises aid in regaining mobility and strengthening the muscles around the ankle, helping to prevent chronic ankle instability without causing excessive strain. Remember, the pace should be guided by pain, and any movement that causes increased pain should be avoided.
Progressive Strengthening Techniques
Progressive strengthening is a key step in the recovery process, encouraging the building of strength over time. Towel curls are recommended as the first of the strengthening exercises after a normal range of motion returns in a healing ankle.
Towel curls are performed by sitting and using the toes to pull and push a towel on the floor. This can be repeated 3 to 5 times a day to strengthen foot muscles. To stimulate and strengthen the plantar fascia, use a golf ball to gently roll under the foot’s arch and pick up marbles with the toes to condition the plantar flexors.
Once these exercises are mastered, progress to isometric exercises, such as pushing the foot against a sturdy object. Then, introduce elastic stretch band exercises for dorsiflexion and plantar flexion to further strengthen the anterior tibialis and gastrocnemius-soleus complex.
Flexibility and Calf Muscle Care
A key component of ankle sprain recovery is maintaining flexibility and caring for your calf muscles. Regular stretching should be done daily, especially before and after any physical activity, to prevent stiffness and reinjury of the calf muscles.
Seated and standing calf stretches enhance the flexibility of the calf muscles during recovery from a sprained ankle. These can be performed with feet shoulder-width apart, toes forward, back straight, shoulders back and down, raising the heels, with extended but not locked knees.
To perform a seated calf stretch, sit with a straight back and core engaged, place feet flat on the ground, and press down on the balls of the feet, lifting the heels. Using a step or stair for calf raises can enhance the stretching range of motion, allowing for a deeper stretch.
Begin stretching the Achilles tendon when it is possible to do so without pain.
Balance and Proprioception Workouts
Balance and proprioception workouts also play a crucial role in ankle sprain recovery. These exercises should start when a patient can stand without pain, provided they were steady on their feet before the injury.
Establishing proprioception and ankle stability can begin with:
- Single-leg balances near a support surface
- Balancing on a wobble board
- Using an ankle disk
- Balancing on one leg with the ankle inverted
Ankle rhythmic stabilization is a technique aimed to improve balance and control as part of a comprehensive ankle rehabilitation process. As rehabilitation progresses, individuals may start with simpler variations of balancing tasks and gradually introduce more challenging variations as their strength and stability improve.
Assessment of postural stability is essential during the rehabilitation process, providing valuable feedback for progress and exercise adjustment.
Advanced Functional Training
Advanced functional training is a step up from basic exercises, providing a more dynamic approach to recovery. Heel raises, for example, enhance calf muscle strength by lifting the heel as high as possible while keeping the knee straight. Heel raises are performed by standing behind a chair for support, rising onto the toes, and gradually lowering back down without favoring the injured side. Once basic heel raises are mastered, a squat variation that targets calves and dynamic ankle stability can be integrated into the exercise regime.
The Y-Balance exercise is a challenging movement that enhances balance, proprioception, and strength by moving the ankle through variable positions. Forward and lateral BOSU lunges combined with single-leg balancing enhance dynamic stability and confidence in the rehabilitated ankle.
Lateral hop and stick exercises are useful in enabling control of lateral movements, and vital for regained stability in the ankle post-sprain.
Utilizing Supportive Gear
Supportive gear, such as ankle braces and taping, can provide additional stability during the recovery process. Ankle bracing during the early stages of rehabilitation can improve proprioceptive feedback and potentially reduce the risk of re-injury.
The lateral ankle stability tape technique can provide feedback on ankle position and improve proprioception after a sprain. It’s essential to choose ankle braces based on the user’s shoe size or ankle circumference to ensure the proper fit and support.
There are various types of ankle braces, each providing a different level of support and comfort. Lace-up ankle braces allow users to adjust tightness for maximum support and a customized fit. Neoprene material in ankle braces provides both support and heat insulation, beneficial for pain, but may not be suitable for all-day use due to lack of breathability.
Fabric and knit ankle braces offer better breathability, keeping the feet cooler, and might be preferable for extended wear. Strap-enhanced ankle supports offer advanced protection by allowing customizable compression levels and are typically available in figure 8 or figure 6 configurations.
Reinforcing Safe Practices
Safe practices are paramount in the recovery process. Pain should guide the pace of rehabilitation exercises for a sprained ankle. It’s crucial to listen to the body’s response to injury, which should dictate the rehabilitation approach for future function and athletic performance.
A personalized rehabilitation program should be constructed based on empirical evidence and knowledge from structured rehabilitation protocols. Kevin D. Plancher advises a cautious approach to recovery, emphasizing the importance of a gradual return to normal activities. The focus should always be on safety and effective recovery.
Recovery Tips from a Sports Medicine Expert
Today’s guide to ankle sprain recovery is informed by the expertise of Kevin D. Plancher, an orthopaedic surgeon and sports medicine expert. With his extensive medical education including a Doctorate in Medicine and a Master’s in Science in Physiology, complemented by an MPH, Kevin D. Plancher’s clinical insight is backed by a strong academic foundation.
His roles as a Clinical Professor at Montefiore Medical Center/Albert Einstein College of Medicine and an Adjunct Clinical Assistant Professor at Weill Cornell Medical College, Cornell University signify his standing in the medical community. Through his leadership at Plancher Orthopaedics & Sports Medicine and his establishment of the non-profit Orthopaedic Foundation for Active Lifestyles, Kevin D. Plancher has extended his impact to the broader community, promoting health and recovery.
Summary
Recovering from an ankle sprain is a journey, one that requires understanding, patience, and above all, guided exercises. By understanding the specifics of your injury, adhering to a personalized recovery program, and following expert advice, you can navigate this path to recovery effectively and safely. Remember, the journey is not a sprint but a marathon, and each step you take brings you closer to your goal. Contact Plancher Orthopaedics to see how we can further help you with your sprained ankle!
Frequently Asked Questions
What is the first step in ankle sprain recovery?
The first step in ankle sprain recovery is to follow the RICE method – Rest, Ice, Compression, and Elevation – to reduce swelling and manage pain effectively.
What are some examples of gentle range of motion exercises?
Some examples of gentle range of motion exercises include flexing, extending, inward and outward bends, ankle circles, and foot alphabet exercises. These exercises can help improve flexibility and reduce stiffness.
How can supportive gear aid in recovery?
Supportive gear such as ankle braces and taping can improve stability, enhance proprioceptive feedback, and reduce the risk of re-injury, aiding in the recovery process.
What is the role of balance and proprioception workouts?
Balance and proprioception workouts play a crucial role in improving stability and control, which are essential for effective ankle sprain recovery.
Who is Kevin D. Plancher?
Kevin D. Plancher is an orthopaedic surgeon and sports medicine expert specializing in knee, shoulder, elbow, and hand injuries. He is a renowned professional in his field.









 Dr. Kevin Plancher is delighted to announce his membership in the
Dr. Kevin Plancher is delighted to announce his membership in the 
 Dr. Kevin Plancher is honored to to be named a Hip and Knee Surgery Research All-Star and ranked in the top 1% of surgeons nationwide. This distinction acknowledges the substantial and high-quality research contributions I’ve made through co-authored publications. Curated by Avant-Garde Health, the Healthcare Research All-Star lists feature exclusively the top 5% of hospitals and surgeons who are leading the way in innovative research. Learn more at
Dr. Kevin Plancher is honored to to be named a Hip and Knee Surgery Research All-Star and ranked in the top 1% of surgeons nationwide. This distinction acknowledges the substantial and high-quality research contributions I’ve made through co-authored publications. Curated by Avant-Garde Health, the Healthcare Research All-Star lists feature exclusively the top 5% of hospitals and surgeons who are leading the way in innovative research. Learn more at 























 William D. Murrell, MD
William D. Murrell, MD Thomas B. Evely, DO
Thomas B. Evely, DO Clifford Voigt, MD
Clifford Voigt, MD Karthikeyan Chinnakkannu, MD
Karthikeyan Chinnakkannu, MD Max N. Seiter, MD
Max N. Seiter, MD Demetris Delos, MD
Demetris Delos, MD Lauren M. Fabian, MD
Lauren M. Fabian, MD