Wondering how to protect your knees from injury during everyday activities and sports? The key to long-term knee health lies in preventative care for knee injuries. This essential guide provides actionable insights into knee joint mechanics and protection strategies that anyone, from weekend warriors to seasoned athletes, can implement to prevent common knee injuries.
Key Takeaways
- Understanding the knee’s anatomy, particularly the role of the ACL and the shock-absorbing functions of the menisci and articular cartilage, is crucial for preventing injuries and maintaining joint health.
- Maintaining a healthy weight and incorporating appropriate exercise regimens, including non-impact aerobic activities and muscle-strengthening exercises, are key strategies for enhancing knee stability and longevity.
- Selecting proper footwear, mastering correct movement techniques, using protective gear like braces and knee guards, and following recovery and nutritional guidelines are essential to support knee health and prevent injuries.
Understanding Knee Joint Mechanics
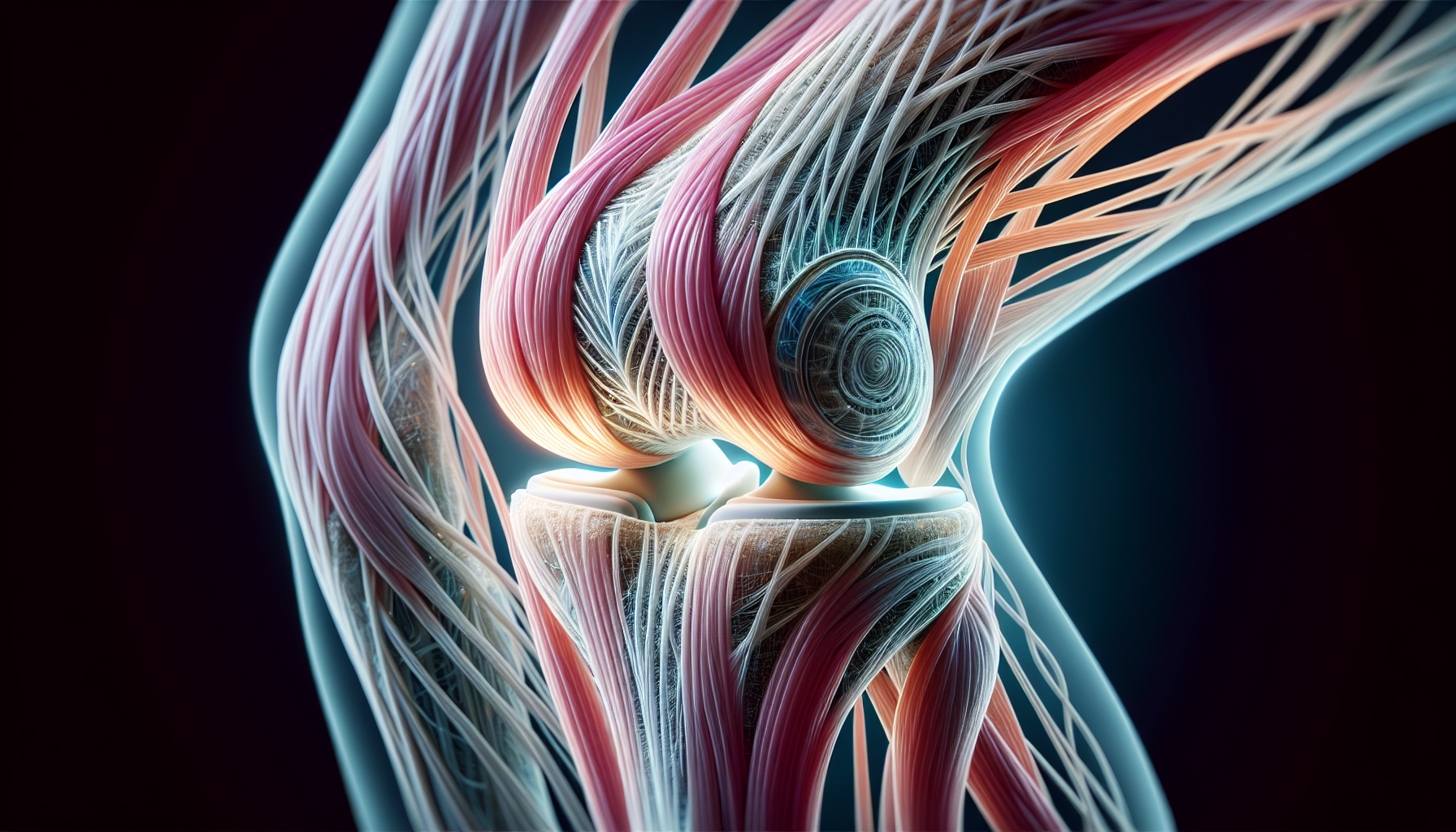
Our knees, often taken for granted, are complex joints that are integral to our everyday movement. From standing up from a chair, walking, running to jumping, our knees bear the brunt of the action. However, the complexity of this joint also leaves it vulnerable to injuries. Sustaining an active lifestyle and preventing long-term mobility issues depend heavily on maintaining knee health. A deep comprehension of the joint’s mechanics is the initial stride to preserving the strength and injury-free status of your knees.
A key player in the knee’s stability and function is the anterior cruciate ligament (ACL). One of the four major ligaments in our knee, the ACL holds the knee together, preventing the tibia from sliding out in front of the femur. Hence, realizing the role of the ACL, its vulnerability to injury, and how it affects knee stability is vital in our path to preserving healthy knees.
Another vital component of the knee joint is the connective tissue and cartilage. These elements act as shock absorbers in our knees, ensuring smooth movement and stability. In the following subsections, we delve deeper into the role of ligaments and connective tissue in knee stability.
The Role of Ligaments in Knee Stability
The ACL plays a crucial role in maintaining knee stability. It prevents the tibia from sliding out in front of the femur and provides rotational stability to the knee. Therefore, any injury to this ligament can severely affect the knee’s stability and function.
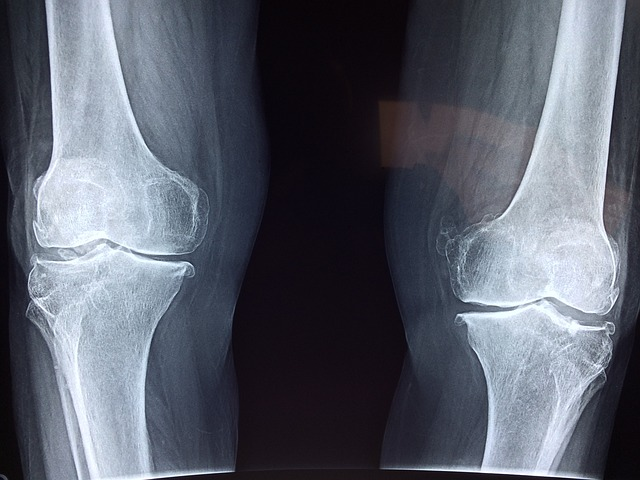
Most ACL injuries result in severe pain and complete or near-complete tears rather than partial ones. These injuries often occur in conjunction with damage to other knee structures such as articular cartilage, meniscus, or other ligaments. This compounds the complexity of the injury and can lead to severe knee pain, and knee problems, and even necessitate a total knee replacement in severe cases.
The complexity of ACL injuries underscores the importance of preventive measures. Comprehending the function of ligaments in knee stability allows us to take measures to prevent knee pain, circumvent knee injuries, and uphold strong, healthy knees.
Connective Tissue and Cartilage: Your Knee’s Shock Absorbers
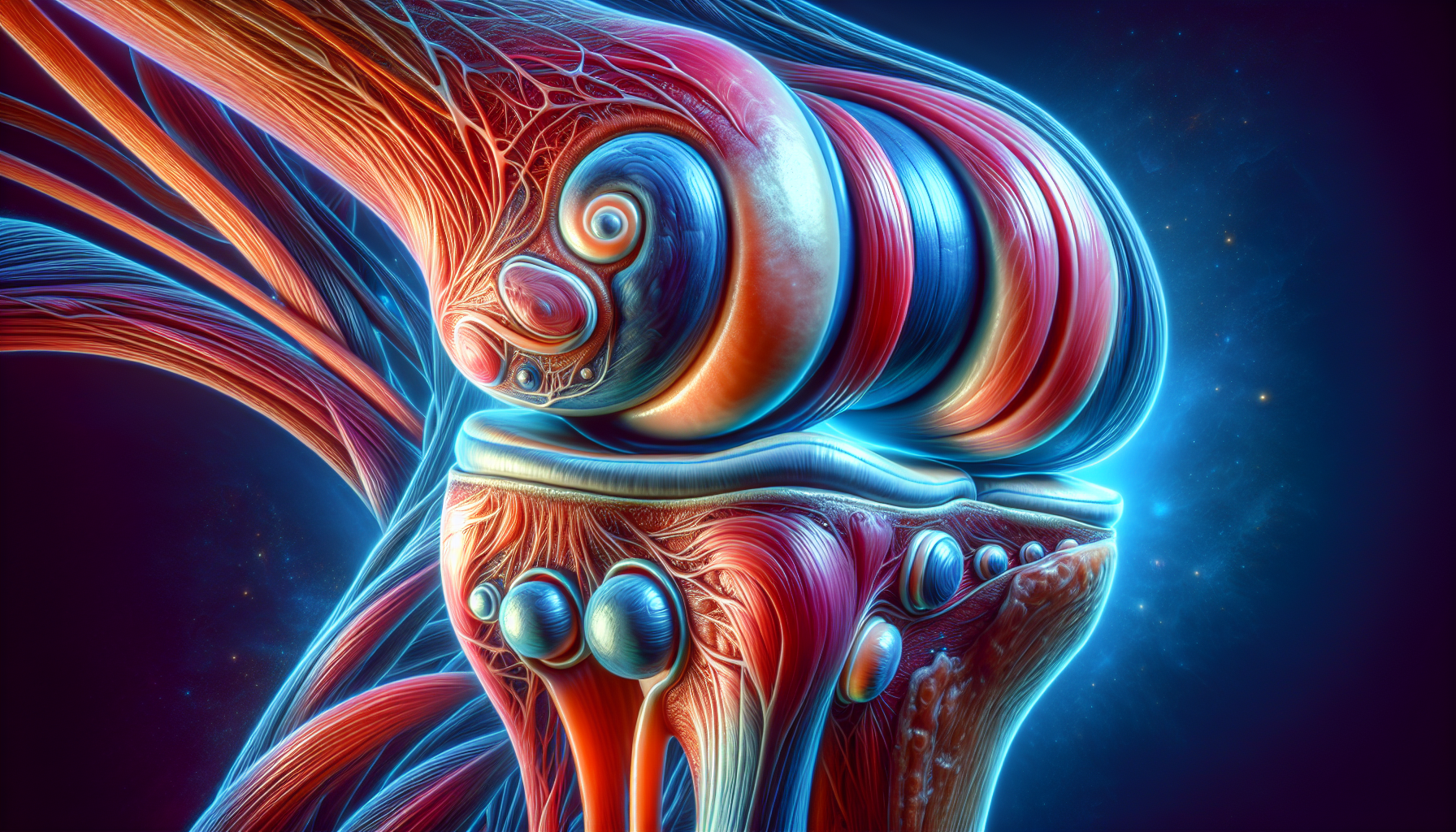
The knee joint’s shock-absorbing function is primarily performed by its menisci and articular cartilage. The knee joint is cushioned by two menisci, with the medial meniscus shaped like a ‘C’ and the lateral meniscus being more circular. These menisci help stabilize the joint by filling the gap between the femur and tibia, preventing the bones from rubbing against each other directly.
Meniscal cartilage can support loads up to 300% of body weight, but its healing is impeded by the limited blood supply, especially within the inner two-thirds known as the ‘white zone’, compared to the more vascular ‘red zone’. This makes the menisci particularly vulnerable to tearing, especially in older adults, leading to common knee injuries and joint pain.
Articular cartilage provides:
- A lubricated, low-friction surface across joint articulations
- Organization in distinct zones and regions to resist compressive and shear forces
- Viscoelastic properties, facilitated by the interaction of chondrocytes in the ECM
- Endurance of high cyclic loads
- Creep and stress-relaxation behaviors, allowing deformation under constant stress and recovery after the stress is removed
Understanding the role of these components in knee joint mechanics can help us take steps to prevent knee injury and keep our knees healthy.
Embracing a Healthy Weight for Knee Longevity
Maintain a healthy weight to ensure knee longevity. Did you know that being only 10 pounds overweight increases the force on the knee by 30-60 extra pounds with each step? This additional force exacerbates the stress on the knee while walking. Hence, upholding a healthy weight is a pivotal element in preventing knee pain and sidestepping usual knee injuries.
Even small amounts of weight loss can significantly with pain management reduce the risk of developing knee osteoarthritis. Losing 10 pounds of weight can result in a 20 percent reduction in pain for individuals with arthritic knees. This emphasizes the importance of weight management in managing knee pain. Hence, shedding weight can not only fortify your knees but also aid in managing knee issues and lessening knee pain.
Being overweight or obese escalates the risk of developing knee osteoarthritis. Overweight women and men are at nearly four and five times, respectively, the risk of developing knee osteoarthritis compared to those at a healthy weight. In the following subsection, we delve deeper into how excess weight impacts knee joints.
The Impact of Excess Weight on Knee Joints
Excess weight significantly impacts knee joints. Being overweight or obese is significantly associated with the development of knee osteoarthritis (OA). This is a concerning fact, given the discomfort and mobility issues associated with osteoarthritis.
Overweight individuals in their thirties, even in the absence of knee OA, have a higher risk of developing the condition later in life. Hence, upholding an active lifestyle and a healthy weight from early on is vital to evade knee injuries and maintain healthy knees.
Weight loss leads to less knee pain and improved walking ability. Specifically, a loss of 20% body weight is associated with considerable pain relief and enhanced mobility in overweight or obese adults. Hence, adopting a healthy weight not only mitigates undue stress on your knees but also enhances your overall health and well-being.
Selecting Footwear to Support Your Knees
The right footwear can make a world of difference when it comes to knee health. Shoes that are comfortable from the moment you try them on are vital since immediate discomfort can indicate poor fit and alignment issues. Hence, when picking shoes, it’s vital to prioritize comfort over style.
Adequate cushioning and support in shoes minimize knee impact, while flexibility and the lack of pressure points ensure a natural walking motion, thus protecting the knees. Hence, when choosing shoes, bear these and other factors well in mind to avert knee pain and safeguard your knees.
Shoes should be replaced when the tread pattern is worn or the heel is unevenly worn, as worn-out soles can lead to improper foot position and increased knee pressure. Hence, stay vigilant for these signs to shield your knees from unnecessary stress.
However, certain types of footwear can do more harm than good, as we will explore in the next subsection.
High Heels vs. Knee Health
High heels, while fashionable, can put extra pressure on the knee joint due to a significant heel-to-toe height difference. Therefore, while they may be perfect for that special occasion, wearing them regularly can lead to knee problems.
Wearing high heels can have negative effects on the knees, including:
- Shifting the body’s weight to the balls of the feet
- Increased pressure on the knee joints
- Stress on knee muscles
- Exacerbation of knee pain
It is important to be mindful of these effects when wearing high heels.
Choosing shoes with a subtle heel-to-toe height difference can help reduce the undue extra stress put on the knees. Hence, it’s advisable to opt for comfort and knee health over fashion when it involves everyday footwear.
Tailored Exercise Regimens for Healthy Knees

Exercise plays a crucial role in maintaining knee health. Regular physical activity is crucial for strengthening the muscles that support the knees, thereby alleviating pain and stiffness in the strongest joints while also aiding in weight management to lessen stress on the knee joints. Hence, integrating an exercise regimen into your daily routine can assist in maintaining strong and healthy knees.
However, it’s critical to avoid high-impact activities that involve repetitive hard impacts or quick pivoting motions, as these can significantly increase the probability of sustaining knee injuries. Hence, selecting the appropriate type of exercise is as significant as the act of exercising.
Incorporating partial squats into an exercise routine offers a functional way to build muscle strength, in the quadriceps, glutes, and hamstrings without imposing excessive strain on the knee joints. In the following subsections, we delve deeper into non-impact aerobic exercises and strengthening exercises that can help maintain healthy knees:
- Walking
- Cycling
- Swimming
- Leg presses
- Step-ups
- Lunges
These exercises can be beneficial for individuals with knee issues or those looking to prevent knee injuries.
Incorporating Non-Impact Aerobic Exercises
Non-impact aerobic exercises like swimming, elliptical workouts, and stationary cycling provide cardiovascular benefits while protecting the knees from harsh impact. Swimming and water-based exercises such as water jogging or water aerobics provide a full-body workout that strengthens the knee joint without harsh impact. Hence, if you aim to diversify your exercise regimen and sustain healthy knees, consider these exercises.
Other effective non-impact aerobic exercises for knee health include elliptical machine workouts and stationary cycling. These exercises provide excellent cardiovascular benefits while having a low impact on your knees. Hence, these exercises can be an excellent inclusion into your exercise routine.
Incorporating short brisk walks and avoiding prolonged periods of intense walking can help maintain an active lifestyle while protecting knee joints from additional stress. Hence, even if workouts aren’t your thing, integrating these minor alterations into your daily routine can significantly contribute to knee health.
Strengthening Exercises: Building Muscle Support
Strengthening leg muscles through specific exercises can significantly reduce the risk of knee injuries and improve joint stability. Hence, including these exercises in your routine can aid in protecting your knees and avoiding injuries.
Hamstring curls, straight leg raises, and side leg raises specifically work on the muscles vital for knee stability. Hence, these exercises can be an excellent supplement to your exercise regimen to keep your knees robust.
Knee extensions and standing knee flexions are targeted exercises to build quadriceps and hamstring strength, thereby supporting the knee joint. Nonetheless, it’s crucial to solicit expert advice on safe weightlifting techniques to prevent inflicting knee pain while attempting to fortify the supporting leg muscles.
Thus, always remember, safety first!
Mastering Movement: Techniques to Prevent Knee Injury

Mastering proper movement techniques can help prevent knee injuries and maintain joint health. Preventing knee injuries is essential and can be achieved through measures such as:
- Proper lifting
- Improving flexibility
- Wearing appropriate shoes
- Strengthening muscles
- Warming up before high-impact activities
- Addressing issues like arthritis or ligament damage
Hence, mastering these techniques can assist you in evading common knee injuries and maintaining healthy knees, ultimately helping you avoid knee pain.
Immediate treatment post-knee injury should include RICE (rest, ice, compression, and elevation) to reduce swelling and promote healing. Hence, if you ever endure a knee injury, it’s vital to recall these steps and implement them promptly.
Incorporating stretching exercises like the standing quadriceps stretch and the pretzel stretch can reduce hip or knee pain and improve flexibility. Hence, stretching should be integrated into your daily routine to uphold muscle elasticity and avert potential injuries.
However, it’s not just about stretching and exercise; maintaining good posture is equally critical, as we will explore in the next subsection.
The Importance of Good Posture
Maintaining good posture is essential for reducing pressure on the knees and contributing to overall joint health. Hence, whether you’re stationed at your desk or out for a run, always keep in mind to uphold good posture.
To prevent knee injuries, it’s important to ensure proper leg alignment by walking and sitting with the head squarely above the shoulders and shoulders directly above the core. This alignment reduces the pressure on your knees and helps maintain joint health.
Maintaining good posture is not just about standing tall. It’s about aligning your body in a way that reduces stress on your joints and muscles. Hence, always ensure to check your posture, be it sitting, standing, or even lying down.
Proactive Measures: Braces and Knee Guards
Wearing braces and knee guards during physical activities can provide additional support and stability for the knee joint, reducing the risk of injuries. Hence, whether you’re out for a jog or engaged in a soccer game, keep in mind to safeguard your knees with braces or knee guards as a part of sports medicine practices.
Prophylactic braces are specifically designed to prevent injuries during contact sports by providing additional knee support, which is crucial for athletes in high-impact sports such as football. Hence, if you’re an athlete, consider employing prophylactic braces for knee protection and averting common knee injuries.
Knee guards and braces offer increased joint stability for individuals with weak or previously injured knees, contributing to increased endurance and power and allowing for movement without fear of re-injury. Hence, if you’ve previously sustained a knee injury, using knee guards or braces can assist you in recovery and preventing further damage.
Recovery Strategies: Physical Therapy and Rest
Implementing recovery strategies like rest, physical therapy, and the RICE method can promote healing and prevent further knee injuries. Rest and sleep are vital for knee injury recovery, as these periods allow for the body’s tissue repair, muscle growth, and natural healing processes. Hence, if you’ve endured a knee injury, remember to grant your body the rest it requires for recovery.
Incorporating recovery strategies such as active rest, compression therapy, and taking breaks enhances the recovery process, prevents knee injuries, and reduces the risk of overuse injuries through adequate recovery of knee joints. Hence, even amid recovery from a knee injury, stay active but also remember to take breaks and permit your body to heal.
Immediate treatment post-knee injury should include RICE (rest, ice, compression, and elevation) to reduce swelling and promote healing. Hence, if you ever endure a knee injury, it’s vital to recall these steps and implement them promptly.
Nutritional Supplements and Joint Health
Nutritional supplements like glucosamine and chondroitin, along with a diet rich in calcium and vitamin D, can support joint health and alleviate pain associated with knee osteoarthritis. Glucosamine and chondroitin supplements are derived from natural components of cartilage and may help with reducing pain, stiffness, and swelling associated with knee osteoarthritis. Hence, if you’re grappling with knee osteoarthritis, consider consulting your healthcare provider about these supplements.
However, it is crucial to consult with a healthcare provider before initiating any supplement regimen for joint health as supplements can have side effects, interact with medications, and should supplement but not replace proven medications. Hence, always seek advice from your healthcare provider before initiating any new supplement regimen.
Maintaining bone health with a diet rich in calcium and vitamin D is imperative for supporting healthy joints, including those in the knee. Hence, don’t forget to incorporate calcium and vitamin D-rich foods in your diet to uphold bone health and strengthen your knees.
Summary
In conclusion, maintaining knee health is a multifaceted approach that involves understanding knee joint mechanics, maintaining a healthy weight, choosing the right footwear, incorporating a tailored exercise regimen, mastering movement techniques, using braces and knee guards, implementing recovery strategies, and taking the right nutritional supplements. By following these guidelines, you can prevent knee injuries, alleviate knee pain, and maintain an active lifestyle. Remember, your knees are crucial to your mobility, and taking care of them today ensures a healthier and happier tomorrow. If you are experiencing a knee injury, contact Plancher Orthopaedics today to see how we can help you!
Frequently Asked Questions
How do you prevent cartilage loss in the knee?
To prevent cartilage loss in the knee, it’s important to engage in low-impact aerobic exercise, strengthening exercises, daily stretching, and maintaining a healthy weight. These measures can help reduce excess wear and tear on the knee cartilage.
What are 3 exercises to strengthen your knee?
Here are 3 exercises to strengthen your knees: knee extension, knee flexion (standing), and heel and calf raises. These exercises can help improve the strength and stability of your knees.
What can I do to prevent knee injuries?
To prevent knee injuries, maintain a healthy weight, wear the right shoes, rethink your exercise routine, add weight training, keep stretching, use proper technique, wear knee guards, and avoid overtraining. These tips can help reduce the risk of knee injuries.
What is the role of the ACL in knee stability?
The ACL is crucial for knee stability as it prevents the tibia from sliding out in front of the femur and provides rotational stability to the knee. It plays a key role in maintaining the structural integrity of the knee joint.
How does excess weight affect knee health?
Excess weight increases the force on the knee joints, worsening pain and raising the risk of conditions like osteoarthritis. It’s important to maintain a healthy weight to protect knee health.












 Greenwich Magazine included Dr. Plancher in their list of Top Doctors 2024. Utilizing information from DataJoe Research, publisher Moffly Media compiled a comprehensive list of the best physicians in Fairfield County.
Greenwich Magazine included Dr. Plancher in their list of Top Doctors 2024. Utilizing information from DataJoe Research, publisher Moffly Media compiled a comprehensive list of the best physicians in Fairfield County.








 Kevin D. Plancher, MD, MPH, FAOA, FAOS attended two conferences in Florida over the past week. On his first stop Dr. Plancher participated in Shoulder360: The Comprehensive Shoulder Course April 13–15, 2023 in Miami Beach. While in attendance as faculty, Dr. Plancher presented “How to Manage the Cuff Patient with Unrealistic Expectations” and participated as a panelist for “Complex Cuff Cases with Non-Arthroplasty Solutions”.
Kevin D. Plancher, MD, MPH, FAOA, FAOS attended two conferences in Florida over the past week. On his first stop Dr. Plancher participated in Shoulder360: The Comprehensive Shoulder Course April 13–15, 2023 in Miami Beach. While in attendance as faculty, Dr. Plancher presented “How to Manage the Cuff Patient with Unrealistic Expectations” and participated as a panelist for “Complex Cuff Cases with Non-Arthroplasty Solutions”.



 Kevin D. Plancher, MD, MPH, FAOA, FAOS is a board-certified orthopaedic surgeon and founder of Plancher Orthopaedics & Sports Medicine. Dr. Plancher is a Clinical Professor, Department of Orthopaedic Surgery, at Montefiore Medical Center/Albert Einstein College of Medicine and an Adjunct Clinical Assistant Professor of Orthopaedic Surgery, at the Weill Cornell Medical College, Cornell University in New York. Since 2001, he has been listed annually in the Castle Connolly directory as a “top doctor” in his field.
Kevin D. Plancher, MD, MPH, FAOA, FAOS is a board-certified orthopaedic surgeon and founder of Plancher Orthopaedics & Sports Medicine. Dr. Plancher is a Clinical Professor, Department of Orthopaedic Surgery, at Montefiore Medical Center/Albert Einstein College of Medicine and an Adjunct Clinical Assistant Professor of Orthopaedic Surgery, at the Weill Cornell Medical College, Cornell University in New York. Since 2001, he has been listed annually in the Castle Connolly directory as a “top doctor” in his field.


 William D. Murrell, MD
William D. Murrell, MD Thomas B. Evely, DO
Thomas B. Evely, DO Clifford Voigt, MD
Clifford Voigt, MD Karthikeyan Chinnakkannu, MD
Karthikeyan Chinnakkannu, MD Max N. Seiter, MD
Max N. Seiter, MD Demetris Delos, MD
Demetris Delos, MD Lauren M. Fabian, MD
Lauren M. Fabian, MD