After suffering a knee injury and going into surgery, swift and effective rehab is crucial for regaining your strength and mobility. This to-the-point guide cuts through the confusion to highlight key steps and exercises in the rehab after knee surgery, equipping you with the knowledge to recover with confidence. Expect to find focused advice on rebuilding your knee’s capabilities and returning to everyday life with greater ease.
Key Takeaways
- Rehabilitation is critical after knee surgery to regain mobility and strength, with the potential for most patients to return to activities within three months if they adhere to a dedicated physical therapy regimen.
- Physical therapy for knee rehab should begin immediately after surgery to prevent complications and starts with pain management, ice therapy, and early assisted mobilizations such as walking to promote healing.
- A personalized rehab plan created by a physical therapist is essential, involving exercises to improve range of motion and strength, self-monitoring progress, setting realistic goals, and a long-term commitment to low-impact activities to maintain knee health post-recovery.
The Importance of Rehabilitation Following Knee Surgery
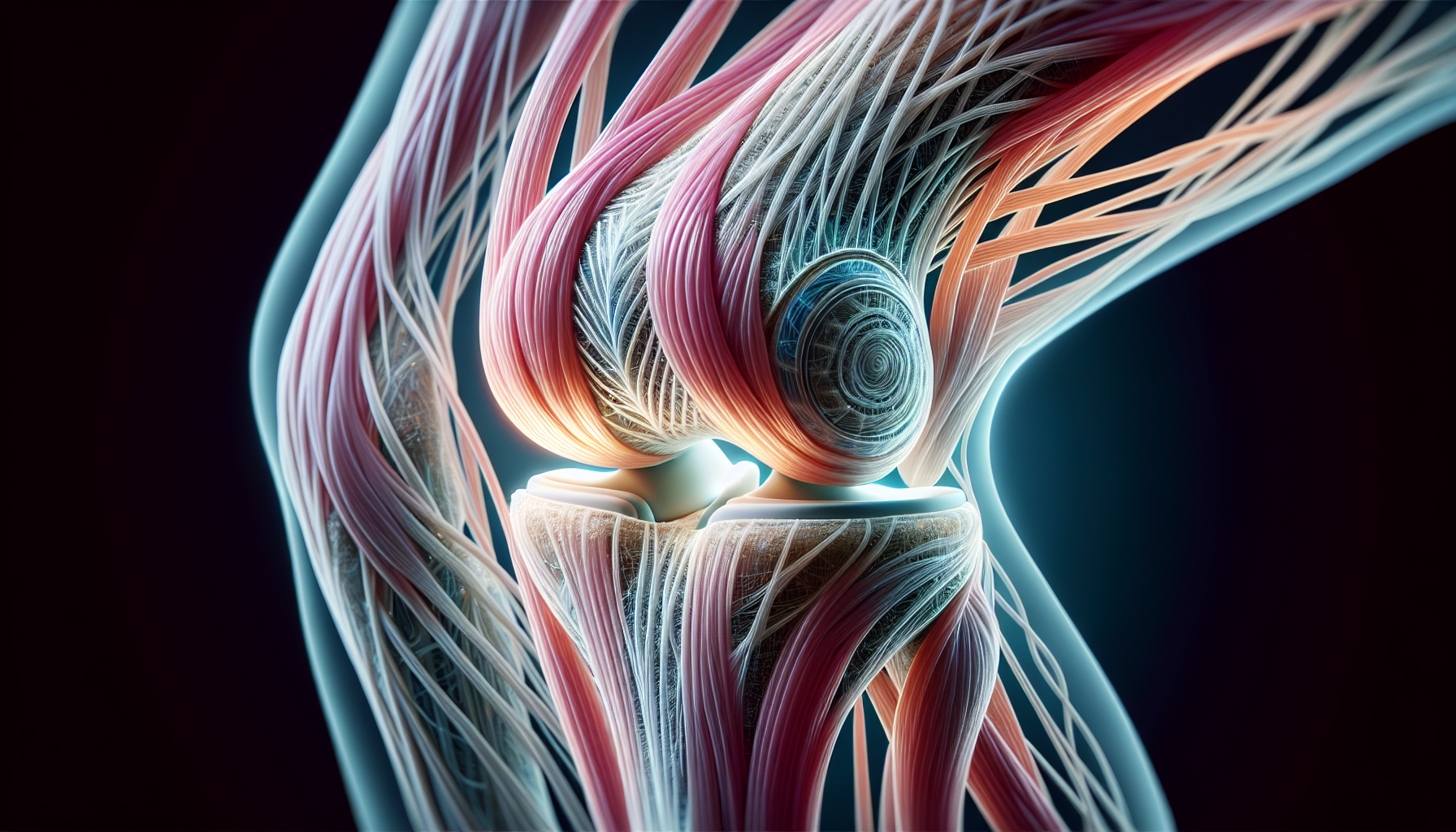
Undergoing knee surgery, including total knee replacement surgery, is just the first step in your journey to reclaiming your mobility. The real magic happens during the rehabilitation phase after joint replacement. Your new knee needs to be trained to function optimally, and that’s where rehabilitation comes into play.
Eliminating knee pain and regaining mobility are the core objectives of an effective rehabilitation plan after knee surgery. And, if you’re worried about the duration of this journey, here’s the good news – engaging in physical therapy exercises and adhering to your doctor’s instructions can significantly speed up your recovery time. In fact, with effective rehabilitation, you can return to most activities in just three months following knee surgery.
Benefits of Rehab
So, what exactly are the benefits of a rehabilitation program after knee surgery? Well, the first goal is to ensure more complete joint movement and safely stimulate the muscles attached to the knee. This is critical to eliminate joint and muscle stiffness, build strength, improve balance, and regain a normal gait.
Physical therapy exercises not only restore mobility, range of motion, and overall joint function following exercises but also strengthen supporting muscles and eliminate stiffness. This means that you’ll not only recover faster but also return stronger. A consistent physical therapy routine after surgery is vital to strengthening supporting muscles and eliminating stiffness.
Whether it’s returning to work or resuming your favorite sport, activity-specific rehabilitation during physical therapy helps restore the strength and skills needed.
The Role of Physical Therapy
Physical therapy is not a one-size-fits-all approach. Every individual is unique, and so are their needs and limitations. This is why physical therapists create a customized rehab program tailored to your specific needs. This could involve a range of exercises that evolve as you progress in your recovery.
Physical therapy techniques such as joint and soft tissue mobilization are used to alleviate pain, improve motion, and aid in healing. Physical therapy plays a pivotal role in accelerating recovery by easing pain, reducing inflammation, maintaining circulation, and restoring joint strength and mobility.
The success of your knee rehabilitation, however, requires your active involvement and adherence to the prescribed program. After all, the goal of physical therapy for knee rehabilitation is not only to restore strength but also to improve overall function and quality of life.
First Steps in Post-Surgery Recovery
Once your surgery is over, and you’re slowly waking up from the anesthesia, you might be wondering, “What’s next?” The first steps in your post-surgery recovery journey involve effective pain management, ice therapy to reduce swelling, and importantly, early mobility. Yes, you read that right! Your rehabilitation begins right after you wake up from surgery, with exercises starting in the recovery room to speed up recovery and decrease post-operative pain.
An immediate post-surgery goal is to get you out of bed and walking within a few hours. This early mobility not only promotes healing but also helps reduce the risk of complications such as blood clots. As for the hospital stay, it typically lasts for one night, with most patients being discharged the following day. However, if you’re in good health and have adequate support at home, discharge on the same day of surgery is also possible.
Pain Management Techniques
Post-surgery pain management is a crucial aspect of your recovery journey. It typically involves a combination of opioids, NSAIDs, and local anesthetics, administered according to a doctor’s instructions. Preemptive analgesia, which is administered before surgery, minimizes central and peripheral hypersensitivity and limits postoperative pain.
Pain management in physical therapy includes using modalities such as:
- heat
- cold
- ultrasound
- electric stimulation
to alleviate pain and promote tissue healing. But it’s important to know that while epidural and patient-controlled analgesia can offer effective pain management, they do come with certain risks such as urinary retention for epidurals and the need for careful monitoring with PCA. So, it’s crucial to follow your doctor’s and physical therapist’s guidance to manage pain effectively and safely.
Early Mobility
Knee surgery might limit you momentarily, but that’s not a reason for you to stay in bed. Physical therapy should begin immediately after surgery to prevent blood clots, promote healing, and avoid muscle atrophy. Assisted walking post-surgery is crucial, starting with aids like walkers or crutches, aiming to gradually transition to partial and then full weight-bearing as strength and endurance improve.
The gradual introduction of weight-bearing exercises is essential, with a focus on planning progressive increases in activity levels while maintaining a balance with rest. Achieving full knee extension within the first 48 hours and progressively increasing knee flexion according to the surgeon’s advice are critical early mobility goals post-knee surgery. So, as you can see, early mobility is key to your speedy recovery.
Developing a Customized Rehab Plan with Your Physical Therapist
Remember how we talked about the importance of a customized rehab plan? Well, your physical therapist will work closely with you to develop a plan tailored to your specific needs. This will focus on areas such as:
- strength
- flexibility
- balance
- coordination
There’s a critical window of time in which the range of motion in surrounding muscles around your new joint can be restored. Your rehab plan will guide you through different stages starting with gentle exercises and advancing towards more demanding ones as prescribed by your physical therapist.
The rehab plan isn’t just about what you do in the clinic. It can also include video visits for your physical and occupational therapist to observe your immediate surroundings. This ensures that prescribed exercises are adapted accordingly to enhance recovery at home.
Setting Realistic Goals
Setting realistic goals is a crucial part of your rehab journey. These goals are not just about improving mobility and restoring functional movement, but also about increasing your independence. A key to successful rehab is finding a balance between the desire to regain mobility and the necessity to avoid actions that cause excessive swelling or pain, which may indicate overexertion.
Personal motivation, bolstered by a positive mindset, significantly affects recovery time after knee surgery and is essential for successful rehabilitation. Whether it’s returning to your favorite sport, or simply being able to play with your grandchildren in the park, setting achievable goals that resonate with your interests can heighten motivation and commitment to your exercise regimen post-surgery.
Monitoring Progress
Just like any journey, your rehab journey also requires you to keep a check on your progress. Regular check-ins with your physical therapist are necessary to assess your progress and adjust your rehab plan, ensuring that it remains tailored to your evolving needs. Keeping track of progress through journals or charts can help visualize milestones. There are even apps that record daily exercises and achievements to contribute to your motivation and consistency with your exercise program.
It’s also important to communicate openly with your healthcare team about any struggles or concerns. This leads to tailored advice and adjustments in the rehab plan to address individual needs. So, don’t hesitate to share your feelings and doubts with your therapist. They’re here to help you.
Essential Exercises for Knee Surgery Rehab
Now, let’s talk about the heart of your rehabilitation plan – the exercises. The initial phase of post-knee surgery rehab focuses on activities designed to improve your range of motion. Then, comes strength training exercises like Quadriceps Sets, Straight Leg Raises, and Knee Straightening Exercises.
As your strength and stability improve, the exercise regimen advances to include more challenging exercises that require standing on one or both feet. After a month of sticking to your rehab schedule, you can expect a dramatic improvement in knee strength and range of motion. And, of course, gait training is incorporated to adjust your walking patterns and reduce the risk of additional knee stress or injury.
Leg Strengthening Exercises
Strengthening your lower leg and muscles plays a crucial role in your recovery. Recommended exercises include:
- Quadriceps Sets
- Straight Leg Raises
- Gluteal Sets
- Short Arc Quads
- Hamstring Raises
These knee-strengthening exercises help build muscle strength and support knee movement, as well as strengthen the supporting muscles around the knee.
As you progress in your recovery, resistance exercises like assisted knee bends and using light ankle weights are introduced to further promote knee strength. Stationary cycling can aid in regaining muscle strength and knee mobility, with a focus on pedaling backward initially and increasing tension over time. Remember, progression in exercises must be gradual to prevent complications and ensure proper recovery.
Range of Motion Exercises
To improve your knee’s range of motion exercises such as Ankle Pumps are recommended. These involve moving the foot up and down to prevent blood clots. Heel Slide exercises, which include sliding the heel towards the legs and buttocks and holding the position, aid in increasing knee flexibility shortly after surgery.
Bed-Supported Knee Bends and Knee Straightening Exercises help initiate the return of mobility and should be performed as soon as possible post-surgery. More advanced exercises like Sitting Supported Knee Bends and Sitting Unsupported Knee Bends further the range of motion by actively bending the operated knee. Focusing on achieving full knee extension and increasing knee flexion is crucial during the first 48 hours following surgery.
Balance and Stability Exercises
Balance and stability are as important as strength and flexibility. For this, your rehab plan will include balance exercises along with proprioceptive training and neuromuscular re-education. Initial balance exercises include standing with one foot on a chair to challenge stability and strengthen leg muscles.
As you advance, you can progress to:
- Standing on your operated leg, which improves stability and core strength
- Balancing on one foot with your eyes closed to better prevent falls (more advanced proprioceptive training)
- Dynamic activities like walking heel-to-toe, are beneficial for coordinating movement and regaining confidence in walking after surgery.
Tips for a Successful Rehab Journey
Embarking on your rehab journey can seem daunting, but there are some things you can do to make it successful. Establishing a new routine during recovery, including set times for personal care, meals, and exercises, can provide comfort and structure, aiding in maintaining motivation.
Staying Consistent with Your Exercise Program
Consistency is key when it comes to your exercise program. Your physical therapist will educate you on the importance of adhering to your rehab program to ensure successful recovery. You can pair exercises with enjoyable activities, such as watching TV or listening to music, to improve adherence to the rehabilitation process.
Patients are recommended to perform their exercises twice a day, with 10 repetitions each session, to maintain consistency in their recovery routine. For continued benefits, patients should persist with their prescribed exercise program at least two to three times a week until eight to ten months post-operation. Incorporating virtual or real rewards can act as a motivational tool to help maintain consistent exercise habits after surgery.
Listening to Your Body
Listening to your body is just as important as sticking to your rehab program. Taking breaks when experiencing pain and stiffness can prevent discouragement and help maintain focus on recovery. If rehab exercises cause severe pain, it is essential to cease these activities and speak with a healthcare professional.
It is important to consult with a doctor before starting any new activities after knee surgery to avoid exacerbating any issues. So, pay attention to your body’s signals and take action accordingly.
Seeking Support
Recovery is often a team effort. Physical therapists may instruct family members or caregivers on how to support you through exercises, ensuring safety and aiding recovery. Joining support groups, like the ACL Recovery Club, can provide the emotional support of a community during rehab.
Some ways to stay connected and receive support during the recovery process include:
- Finding a ‘rehab buddy’ who can provide direct support and encouragement by sharing experiences and participating in exercises
- Accepting help from family and friends for tasks and errands, as it is not a sign of weakness
- Staying connected with others and making friends in physical therapy
- Staying in touch with loved ones to help prevent feelings of isolation and depression during recovery.
Long-Term Recovery and Maintaining Knee Health
Once you’ve completed your rehab program, the journey doesn’t end there. Adherence to exercise routines post-rehabilitation can lead to a return to normal daily life with minimal limitations on high-impact activities.
By 12 weeks post-surgery, most patients should be able to participate in low-impact recreational activities such as walking and swimming, with significantly reduced stiffness and pain.
Continuing Exercises
Continuing with the prescribed exercises post-rehab is vital for maintaining the benefits achieved during the rehabilitation process. Regular follow-up appointments during the first year after knee surgery are key to ensuring ongoing improvement in knee and overall health afterwards.
Engaging in Low-Impact Activities
Engaging in low-impact activities like walking, swimming, and cycling promotes weight management and knee joint longevity. Walking aids in building knee strength and can be incrementally increased in difficulty.
Swimming and water exercises offer non-weight-bearing movement that minimizes stress on the artificial knee.
Summary
In this comprehensive guide, we’ve unveiled the key aspects of a successful rehabilitation journey after knee surgery – from the importance of rehab to the role of physical therapy, from pain management techniques to early mobility, from setting realistic goals to monitoring progress, and from essential exercises to tips for a successful rehab journey. Remember, your active involvement and adherence to the prescribed rehab program play a pivotal role in your recovery.
As Dr. Kevin D. Plancher, an experienced orthopedic surgeon, always says, “Rehabilitation after knee surgery is not a sprint, it’s a marathon.” So, be patient, stay consistent, listen to your body, seek support, and keep moving forward, because every step you take is a step closer to reclaiming your mobility and getting back to the activities you love. Contact Plancher Orthopaedics today to learn more information!
Frequently Asked Questions
How long is rehab after knee surgery?
Rehabilitation after knee surgery typically lasts about 12 weeks, but many people can walk without assistance after 3 weeks and drive after 4–6 weeks. Most patients can take care of themselves within 3 to 6 more weeks after surgery.
What is the hardest part of knee replacement recovery?
The hardest part of knee replacement recovery is regaining knee motion in the early stages, up to 3 months postoperative. This can be a significant challenge for many patients.
What are the do’s and don’ts after knee surgery?
After knee surgery, avoid downhill skiing or contact sports like football and soccer. Instead, opt for lower-impact activities such as hiking, gardening, swimming, tennis, and golf.
How long does it take for a knee to fully heal after surgery?
It may take around 4 to 6 months, or up to a year, to fully recover after knee replacement surgery, depending on various factors such as activity level before surgery.
What exercises are recommended after knee surgery?
After knee surgery, it’s important to do exercises like Quadriceps Sets, Straight Leg Raises, and Knee Straightening Exercises to build muscle strength and support to bend your knee during movement. These exercises can aid in the recovery process.










 Dr. Kevin Plancher attended the American Academy of Orthopaedic Surgeons (AAOS) 2024 Annual Meeting this week in San Francisco. While in attendance, Dr. Plancher presented Office-Based Arthroscopy: Shoulder and Knee during the Office-Based Orthopaedic Surgery: Open, Arthroscopic, and Ultrasound-Guided moderated by Shaft Sraj. Dr. Plancher joined John G. Kennedy in discussing the advances made by adopting the office as a surgical setting, as compared to wide-awake surgery which is defined by the choice of anesthesia. They also demonstrated various application in shoulder, hand and elbow, as well as foot and ankle surgery, including US-guided surgery.
Dr. Kevin Plancher attended the American Academy of Orthopaedic Surgeons (AAOS) 2024 Annual Meeting this week in San Francisco. While in attendance, Dr. Plancher presented Office-Based Arthroscopy: Shoulder and Knee during the Office-Based Orthopaedic Surgery: Open, Arthroscopic, and Ultrasound-Guided moderated by Shaft Sraj. Dr. Plancher joined John G. Kennedy in discussing the advances made by adopting the office as a surgical setting, as compared to wide-awake surgery which is defined by the choice of anesthesia. They also demonstrated various application in shoulder, hand and elbow, as well as foot and ankle surgery, including US-guided surgery.









 Greenwich Magazine included Dr. Plancher in their list of Top Doctors 2024. Utilizing information from DataJoe Research, publisher Moffly Media compiled a comprehensive list of the best physicians in Fairfield County.
Greenwich Magazine included Dr. Plancher in their list of Top Doctors 2024. Utilizing information from DataJoe Research, publisher Moffly Media compiled a comprehensive list of the best physicians in Fairfield County.

 William D. Murrell, MD
William D. Murrell, MD Thomas B. Evely, DO
Thomas B. Evely, DO Clifford Voigt, MD
Clifford Voigt, MD Karthikeyan Chinnakkannu, MD
Karthikeyan Chinnakkannu, MD Max N. Seiter, MD
Max N. Seiter, MD Demetris Delos, MD
Demetris Delos, MD Lauren M. Fabian, MD
Lauren M. Fabian, MD