Dealing with knee pain that intensifies when you’re active? Patellofemoral pain syndrome could be the issue. Affecting a wide range of individuals, this condition is not only common but also treatable. In this article, we’ll explore effective ways to ease your knee pain and preventative measures to keep it from hindering your lifestyle.
Key Takeaways
- Patellofemoral Pain Syndrome (PFPS) is commonly caused by structural and functional disruptions in the knee joint and can affect adults and adolescents, requiring a precise diagnostic process and a tailored management plan that can include physical therapy and surgery in severe cases.
- Non-surgical treatments for PFPS such as activity modification, physical therapy, medication, and orthotics can often effectively manage symptoms and improve knee function without the need for surgical intervention.
- Surgical treatment for PFPS may be considered after exhausting non-surgical options, with arthroscopy and tibial tubercle transfer being potential procedures to reduce pain and improve alignment, complemented by ongoing prevention and maintenance strategies such as exercise, appropriate footwear, and weight management.
Understanding Patellofemoral Pain Syndrome

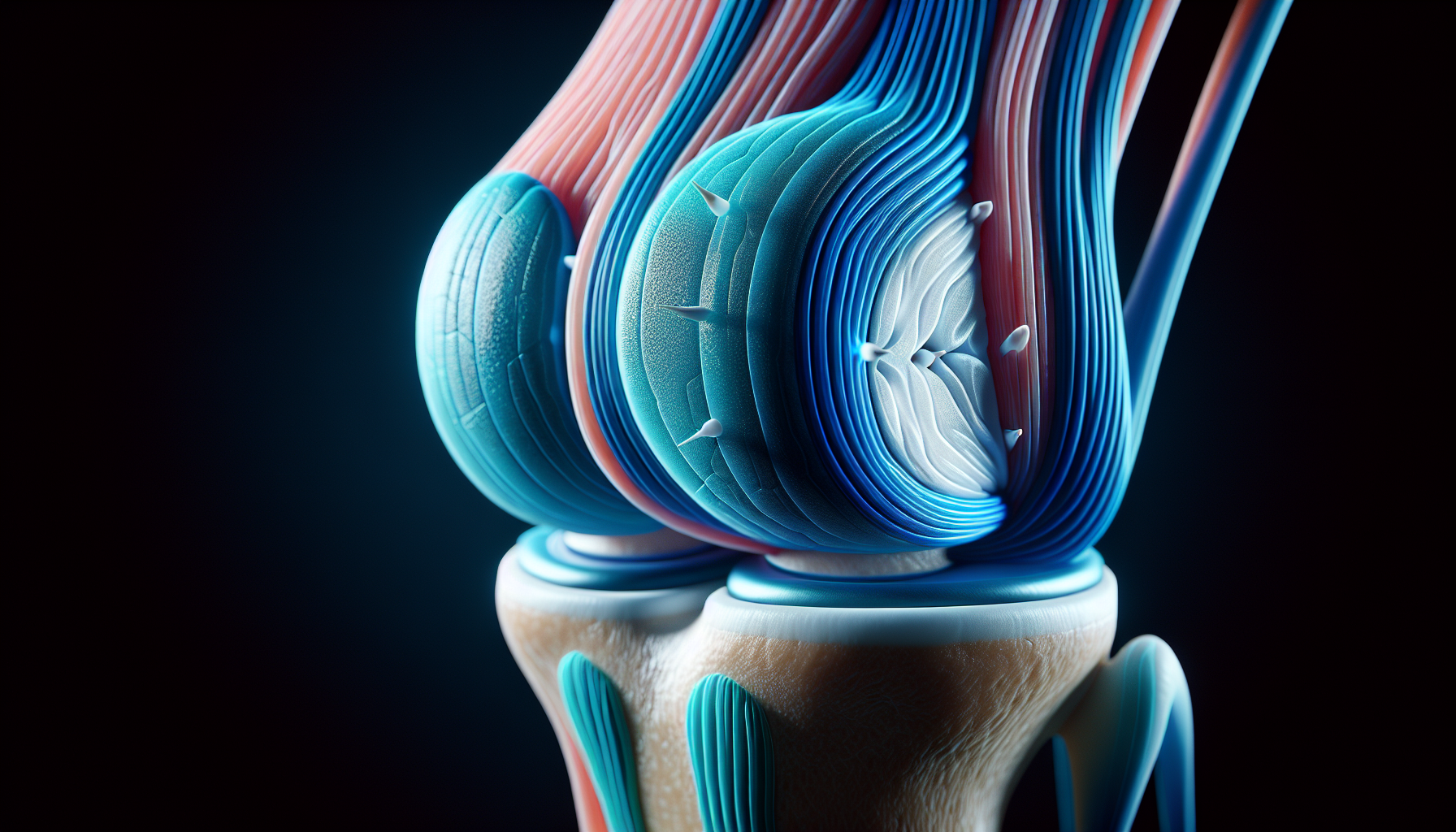
When knee pain begins to put a damper on everyday activities, it’s essential to look beneath the surface and understand what could be at the heart of the issue. Patellofemoral Pain Syndrome (PFPS) is a condition characterized by discomfort originating from the knee joint or surrounding soft tissues, often exacerbated by activities that put stress on the knee, such as squatting, running, or even sitting for prolonged periods. While treating patellofemoral pain syndrome may seem daunting, it is a common ailment, affecting approximately one-quarter of adults and one-third of adolescents, with a noted prevalence in women. The journey to pain relief is a road well-traveled, and with the right knowledge, you can navigate it successfully.
Understanding the nuances of patellofemoral pain, often referred to as anterior knee pain, is critical, as it often presents as an aching pain at the front of the knee, a symptom familiar to many but attributed to various potential causes. The pain may be fleeting or become a chronic companion, and it isn’t picky about whom it affects—both genders across all age groups can find themselves coping with this knee problem. With a clear diagnosis and a comprehensive management plan, including physical therapy and potentially knee surgery for more severe cases, it’s possible to reduce pain and regain the full function of your knee joint. In some cases, individuals may report anterior knee pain encountered during specific activities or movements.
Symptoms and Diagnosis
The common symptoms of patellofemoral pain syndrome tend to be as straightforward as they are inconvenient. A dull, aching pain at the front of the knee, often related to physical activity, can signal that something is amiss within the complex structures of the knee joint. Diagnosing PFPS is a nuanced process that requires a clinical examination to identify signs that point toward this particular pain syndrome. It’s not unusual for a patient to recount the discomfort encountered during actions as simple as climbing stairs or standing up after prolonged sitting, which can further inform a differential diagnosis.
While imaging tests such as MRI or CT scans are not typically necessary for most patients, a physical examination may be considered if there has been trauma, previous knee surgery, or a lack of improvement with standard treatment. A functional evaluation, such as the stair stepping test, provides valuable insights into the knee’s functionality under stress and helps ensure that the diagnosis of PFPS is accurate and that the prescribed treatment will target the right areas for pain reduction.
Causes and Risk Factors
Navigating the root causes of patellofemoral pain syndrome is akin to untangling a complex web, where each strand could be a contributing factor. Some common factors that can lead to PFPS include:
- Anatomical issues like a high-riding kneecap or a shallow groove in the femur
- Lower extremity malalignment that places undue stress on the knee joint
- Weak thigh muscles
- Tight hamstrings
- Tight Achilles tendons
These factors can disrupt the delicate balance of forces acting on the patellofemoral joint, leading to pain and dysfunction that extends beyond the knee and impacts quality of life.
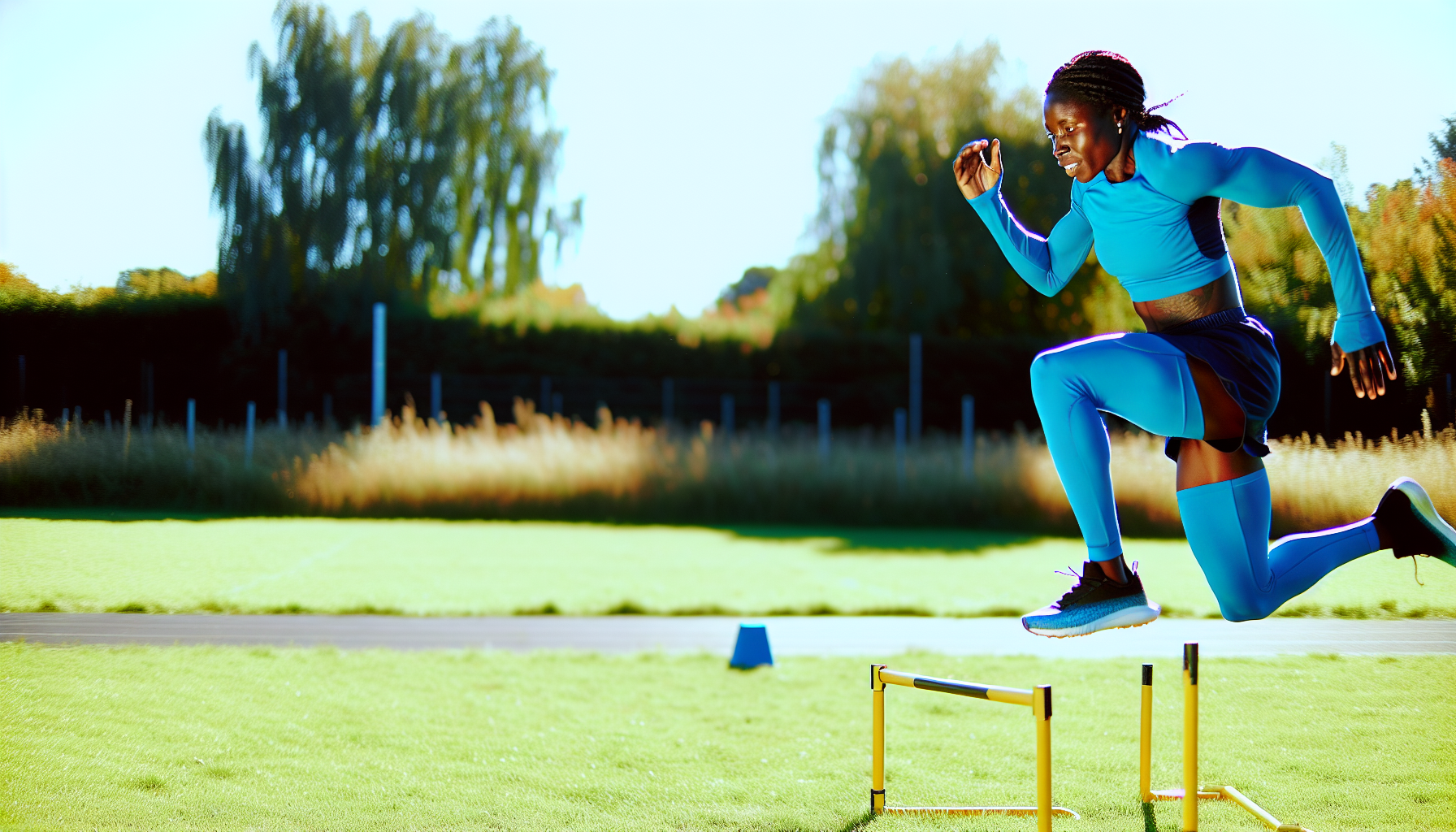
But it’s not just anatomical risks that can lead a person down the path to patellofemoral pain. Overuse injuries, often seen in athletes or individuals who suddenly increase their physical activity levels, are notable triggers. A sudden change in daily activities or footwear can also catapult the knee out of its comfort zone, igniting the onset of PFPS. Even a direct blow or trauma to the knee can set the stage for pain syndrome to emerge, showcasing the need for a broad approach to both treatment and prevention.
Non-Surgical Treatment Options
When confronting patellofemoral pain syndrome, the arsenal of non-surgical treatment options serves as the first line of defense. These treatments include:
- Activity modification
- Medication
- Physical therapy
- Orthotics
These treatments aim to provide pain relief and improve knee function without the need for the surgeon’s scalpel. Even though knee braces are often considered, studies suggest that they may not significantly benefit when combined with physical therapy.
However, by exploring other non-surgical interventions, many find they can manage their symptoms effectively and avoid the complexities of knee surgery.
Activity Modification
Part of mastering the management of patellofemoral pain involves making strategic changes to one’s physical activity. Activity modification is essential, focusing on minimizing stress on the patellofemoral joint to achieve pain reduction. It’s advised to steer clear of high-impact activities that could exacerbate knee pain, like deep squats or lunges, instead embracing low-impact exercises such as stationary biking or swimming.
Such adjustments not only foster a healing environment for the knee but also allow individuals to maintain their fitness levels, a vital component of overall well-being.
Medication
In the quest for pain relief, medication often plays a pivotal role in the management of patellofemoral pain syndrome. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen, along with acetaminophen, are commonly recommended to help alleviate knee pain. While these medications are widely used and can provide a measure of pain relief, it’s important to note that their effectiveness in treating PFPS specifically is not well-established by evidence.
Therefore, medication is typically one component of a broader treatment strategy that includes physical therapy and other non-surgical interventions.
Physical Therapy
Physical therapy stands as a cornerstone in the treatment of patellofemoral pain, guiding patients through a tailored rehabilitation program. A physical therapist will meticulously craft a plan that addresses the strengthening of the quadriceps and core muscles, aiming to improve the knee’s stability and function.
Stretching exercises to improve flexibility in tight lateral structures and poor quadriceps flexibility are also integral to the therapy regimen, helping to correct maltracking of the patella. By focusing on these key areas, physical therapy can offer significant pain reduction and help prevent the recurrence of symptoms.
Orthotics
Orthotics serve as a supportive ally in the battle against patellofemoral pain, offering stabilization and support for the knee joint. Over-the-counter soft orthoses, as well as custom orthotics, can be valuable for those whose symptoms persist despite other treatments.
Knee braces, while helpful for some, especially in the early stages of PFPS, should be considered as an adjunct to exercise therapy and other physical interventions. These devices can help to reduce pain during physical activity, allowing individuals to stay active and engaged in their recovery process.
Surgical Treatment Options
In certain severe cases of patellofemoral pain syndrome, when non-surgical treatments have been exhausted without satisfactory pain relief, surgical options may come into play. These procedures, including arthroscopy and tibial tubercle transfer, are aimed at improving the alignment of the kneecap and relieving the pressure that contributes to pain.
While the thought of knee surgery can be daunting, these interventions are designed to relieve pain, restore functionality, and enhance the quality of life for those suffering from chronic pain, particularly intractable knee pain.
Arthroscopy
Arthroscopy represents a minimally invasive surgical technique that allows orthopaedic surgeons to peer into the knee joint and addresses any underlying issues. Through a small incision and using a camera-equipped device, the surgeon can:
- assess and repair damage within the knee joint
- remove loose bodies or cartilage fragments
- repair torn ligaments or tendons
- remove inflamed synovial tissue
- treat conditions such as arthritis or meniscal tears
This procedure often results in less recovery time and postoperative pain compared to traditional open surgery.
This procedure is particularly useful for severe cases of PFPS where cartilage damage or other internal knee problems need to be corrected to achieve pain relief.
Tibial Tubercle Transfer
For those with PFPS caused by malalignment or articular degeneration, a tibial tubercle transfer can be a transformative surgical option. By repositioning the attachment of the patellar tendon, this technique aims to improve the alignment of the kneecap, thereby decreasing patellofemoral contact stress and balancing forces across the joint. With high subjective and objective success rates, tibial tubercle transfer surgery offers a beacon of hope for those seeking a long-term solution to intractable patellofemoral pain.
Moreover, the procedure has been shown to avoid serious postoperative complications, such as compartment syndrome and infection, in a significant number of cases.
Prevention and Maintenance
The adage “an ounce of prevention is worth a pound of cure” holds particularly true for patellofemoral pain syndrome. By adopting proactive strategies focused on exercise and strengthening, proper footwear, and weight management, individuals can significantly reduce their risk of developing PFPS or manage its symptoms over the long term.
Moreover, understanding the importance of proper technique in physical activities, along with the benefits of gradual increases in intensity, can further aid in the prevention of a runner’s knee, a common knee problem.
Exercise and Strengthening
A well-rounded exercise regimen that includes both hip and knee exercises is recommended for the effective treatment and prevention of patellofemoral pain syndrome. Targeting these areas can enhance knee strength and alleviate discomfort, with specific exercises such as squats and heel raises being particularly beneficial.
Additionally, incorporating stretching into one’s routine at least three times a week can promote flexibility and further aid in the prevention of knee issues.
Proper Footwear and Orthotics
The foundations of knee health can be significantly influenced by the choice of footwear and the use of orthotics. Here are some tips to consider:
- Choose well-fitting, activity-specific shoes with stability support and cushioning
- Avoid shoes with worn-out soles or inadequate arch support
- Consider using orthotics or shoe inserts for additional support and alignment
These measures can help prevent the development of patellofemoral pain syndrome and promote overall knee health.
In cases where additional support is needed, orthotic inserts or custom insoles can provide the necessary arch support to reduce the risk of knee problems. By addressing poor foot support and pronation, individuals can take an active role in safeguarding their knees against PFPS.
Weight Management
Weight management is an often overlooked but critical aspect of knee joint health. Maintaining a healthy weight can significantly reduce the pressure on the knee joint and alleviate the stress that contributes to patellofemoral pain syndrome.
By engaging in regular physical activity and adopting a balanced diet, individuals can better manage their body mass index (BMI) and, in turn, reduce the risk of knee problems.
Summary
As we reach the end of our comprehensive guide to conquering patellofemoral pain syndrome, it’s clear that the road to recovery involves a multifaceted approach. From understanding the symptoms and causes to exploring non-surgical treatments and considering surgical options when necessary, managing PFPS requires patience, knowledge, and a proactive stance. Remember, whether it’s through targeted exercises, the right footwear, or maintaining a healthy weight, the power to reduce pain and prevent future knee problems is within your grasp. Embrace these strategies, and step confidently toward a future where knee pain no longer holds sway over your life. Contact Plancher Orthopaedics today and see how we can help you with patellofemoral pain syndrome.
Frequently Asked Questions
What is the most effective non-surgical treatment for patellofemoral pain syndrome?
Physical therapy is considered the most effective non-surgical treatment for patellofemoral pain syndrome as it focuses on strengthening the quadriceps and core muscles, improving flexibility, and correcting patellar maltracking. This can alleviate pain and enhance knee function.
Can patellofemoral pain syndrome be cured completely?
Patellofemoral pain syndrome cannot be completely cured, but many individuals can achieve significant pain relief and improved knee function through a combination of treatments. Surgery may be necessary in severe cases.
How long does it typically take to recover from PFPS?
Recovering from PFPS can take anywhere from a few weeks to several months, depending on the severity of the condition and the effectiveness of the treatment plan.
Is running bad for patellofemoral pain syndrome?
Running can worsen patellofemoral pain syndrome if not done correctly, but with proper form, footwear, and gradual intensity increase, it can be effectively managed.
Are there any lifestyle changes that can help prevent PFPS?
Yes, maintaining a healthy weight, engaging in regular low-impact exercise, wearing supportive footwear, and incorporating stretching into your routine can help prevent PFPS. These lifestyle changes can significantly reduce the risk of developing PFPS.













 Dr. Kevin Plancher is delighted to announce his membership in the
Dr. Kevin Plancher is delighted to announce his membership in the 
 Dr. Kevin Plancher is honored to to be named a Hip and Knee Surgery Research All-Star and ranked in the top 1% of surgeons nationwide. This distinction acknowledges the substantial and high-quality research contributions I’ve made through co-authored publications. Curated by Avant-Garde Health, the Healthcare Research All-Star lists feature exclusively the top 5% of hospitals and surgeons who are leading the way in innovative research. Learn more at
Dr. Kevin Plancher is honored to to be named a Hip and Knee Surgery Research All-Star and ranked in the top 1% of surgeons nationwide. This distinction acknowledges the substantial and high-quality research contributions I’ve made through co-authored publications. Curated by Avant-Garde Health, the Healthcare Research All-Star lists feature exclusively the top 5% of hospitals and surgeons who are leading the way in innovative research. Learn more at 















 William D. Murrell, MD
William D. Murrell, MD Thomas B. Evely, DO
Thomas B. Evely, DO Clifford Voigt, MD
Clifford Voigt, MD Karthikeyan Chinnakkannu, MD
Karthikeyan Chinnakkannu, MD Max N. Seiter, MD
Max N. Seiter, MD Demetris Delos, MD
Demetris Delos, MD Lauren M. Fabian, MD
Lauren M. Fabian, MD