Are you considering minimally invasive knee arthroplasty techniques for your knee surgery? Understanding these procedures is key to a faster recovery and less pain. Our article, “Minimally Invasive Knee Arthroplasty Techniques: What You Should Know,” dives into the crucial aspects you need to know, from the specifics of the surgical approaches to the benefits they offer. Learn what sets these techniques apart and what to look for in a surgeon, all to help you make a well-informed decision.
Key Takeaways
- Minimally Invasive Knee Arthroplasty (MIKA) techniques, including the Mini-Incision, Quadriceps-Sparing, and Subvastus approaches, are designed to reduce surgery impact, speed up recovery, and minimize pain and tissue disruption.
- Successful MIKA outcomes depend on the expertise of the orthopedic surgeon, which is critical in managing the unique challenges of minimally invasive procedures and ensuring patient satisfaction and quicker recoveries.
- Despite the advantages of MIKA, it entails potential complications like infection and nerve damage, necessitating experienced surgeons and appropriate patient selection to mitigate risks and achieve long-term positive outcomes.
Exploring Minimally Invasive Knee Arthroplasty (MIKA) Techniques
Ever pondered how knee surgery has evolved into more patient-focused procedures? MIKA techniques are the answer, designed to diminish the impact of surgery on the body while ensuring the same, if not better, outcomes compared to traditional methods. These techniques, which utilize smaller incisions and cause minimal tissue disruption, are transforming orthopedic surgeons’ approach to knee joint issues. They address challenges such as:
- limited access and visibility
- longer recovery times
- higher risk of infection
- more post-operative pain
These challenges are circumvented by employing advanced instruments and innovative surgical strategies.
Three distinctive pathways to the knee joint include the Mini-Incision Technique, the Quadriceps-Sparing Approach, and the Subvastus Approach, each tailored to reduce the invasiveness of the procedure.
Mini-Incision Technique
The Mini-Incision Technique is akin to performing intricate artistry through a keyhole — it’s all about precision and minimizing collateral damage. A smaller midline skin incision, ranging from 6 to 14 cm, paves the way for surgeons to reach their canvas — the knee joint. This minimally invasive technique, also known as a minimally invasive surgical technique, aims to achieve the desired surgical outcomes with a significantly smaller cut than traditional surgery, which can mean less soft tissue trauma and a potentially easier recovery path for patients.
Quadriceps-Sparing Approach
Consider the Quadriceps-Sparing Approach as the gentle giant among surgical techniques. It’s designed to avoid slicing through the quadriceps tendon, which is a crucial component of knee strength and function. By sparing this vital tendon, patients may experience less post-operative pain and find themselves back on their feet more quickly than they would with traditional knee replacement surgery.
The intricacy of this approach, however, does not come without its demands; it requires specialized instruments and a surgeon skilled in navigating through the smaller surgical field.
Subvastus Approach
The Subvastus Approach takes a route less traveled, slipping beneath the vastus medialis muscle to reach the knee joint, as opposed to more conventional methods that may cut through or split the quadriceps muscle or tendon. By engaging the vastus medialis obliquus (VMO) muscle, which is part of the quadriceps group, this approach offers a pathway that is both innovative and less invasive.
This approach exemplifies the continual refinement of surgical techniques with the goal of reducing recovery time and enhancing overall outcomes.
Benefits of Choosing Minimally Invasive Techniques
The appeal of minimally invasive techniques extends beyond their name; it’s rooted in the tangible benefits they offer. Enter the operating room with a minimally invasive approach, and you’re likely to leave with a minimally invasive knee replacement, a type of minimally invasive surgery, featuring:
- new knee components
- a smaller scar
- less postoperative pain
- a potentially shorter hospital stay
These advantages align with the goals patients often have when considering knee replacement surgery — to alleviate pain and regain mobility with minimal downtime.
Moreover, studies have shown that the long-term outcomes, such as knee alignment and functionality, are comparable to those of traditional total knee replacement, ensuring that patients enjoy a quality of life that is not compromised by the choice of a less invasive approach over traditional knee replacement.
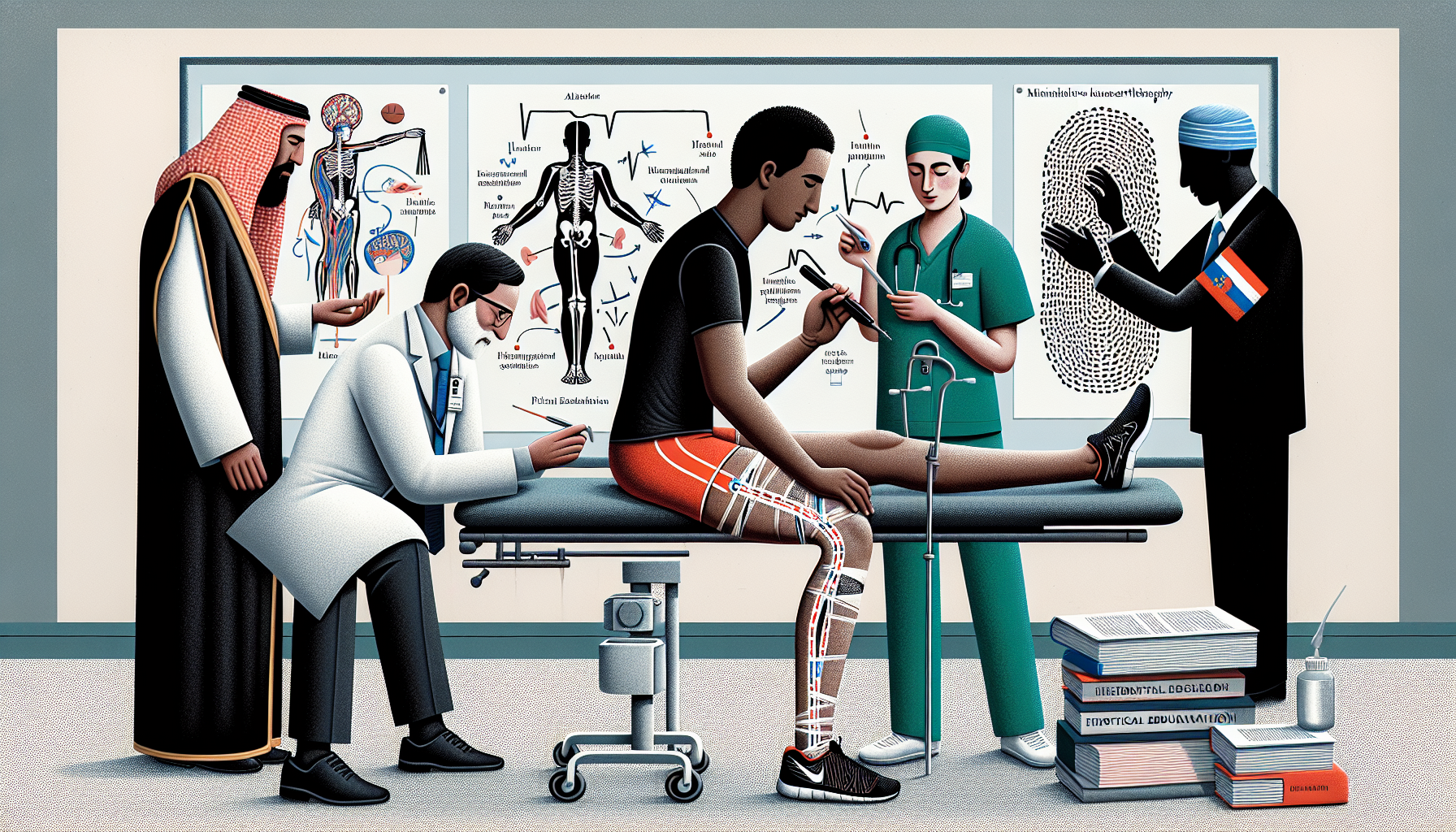
Selecting the Right Orthopedic Surgeon for MIKA
Beginning the knee replacement surgery journey hinges on one crucial step: choosing the appropriate orthopedic surgeon. The expertise of the surgeon you choose can have a profound impact on the success of your MIKA procedure. Factors like board certification, specialized training in joint replacement surgery, and the number of MIKA procedures performed should be considered as they can significantly impact the results of your surgery.
Moreover, engaging in a consultation with potential surgeons provides an opportunity to discuss the specifics of MIKA, allowing you to make an informed decision that suits your unique needs.
Importance of Surgeon Expertise
The expertise of a surgeon is more than just a noteworthy credential; it constitutes a cornerstone of successful MIKA procedures. An experienced surgeon brings a wealth of knowledge and refined skills that translate into better outcomes, quicker recoveries, and a smoother surgical experience for patients. It takes approximately 30 cases for a surgeon to achieve a level of comfort with minimally invasive techniques, which suggests there is a learning curve that leads to improved efficiency and reduced operative time.
Moreover, the expertise of the surgeon becomes even more paramount in cases where patient characteristics, such as obesity or muscular legs, present additional challenges during surgery.
Evaluating Patient Testimonials
Patient testimonials offer a glimpse into the real-world outcomes and satisfaction levels associated with a surgeon’s work. Nonetheless, these narratives should be approached with discernment, acknowledging the source and potential bias that might distort the overall representation. Reviews should be taken as part of a broader assessment, where consistency between patient-reported outcomes and clinical results can lend credibility to a surgeon’s track record.
Keep in mind that while testimonials can be informative, they often lack comprehensive information about patient health and long-term outcomes, which are crucial aspects of the decision-making process.
Preoperative Considerations and Preparation
The preoperative phase, a crucial period of preparation, sets the stage for a smooth surgical journey and optimal recovery. It encompasses a variety of steps, including a thorough medical evaluation to ensure patient safety and readiness for the procedure. Additionally, patients are encouraged to engage in preoperative physical therapy, also known as “prehabilitation,” to strengthen the knee joint and educate themselves about the upcoming surgery and recovery process.
Medical Evaluation
Prior to being approved for surgery, patients are subject to a comprehensive medical assessment, a step of particular importance for those with underlying health conditions like diabetes or heart disease. Routine preoperative tests, including blood counts, coagulation studies, and electrocardiography, are essential for identifying any potential concerns that could complicate the surgery.
Maintaining good cardiopulmonary function is also vital for managing anesthesia and blood loss throughout the procedure.
Physical Therapy and Patient Education
Proactive measures such as physical therapy and education can contribute to lesser postoperative pain and enhanced knee function. Patients who are well-informed and physically prepared tend to experience a smoother recovery and are better equipped to manage the postoperative phase.
Making home preparations, such as arranging for a caregiver and modifying the living space, can significantly contribute to a safe and conducive recovery environment.
The Surgical Procedure Unveiled
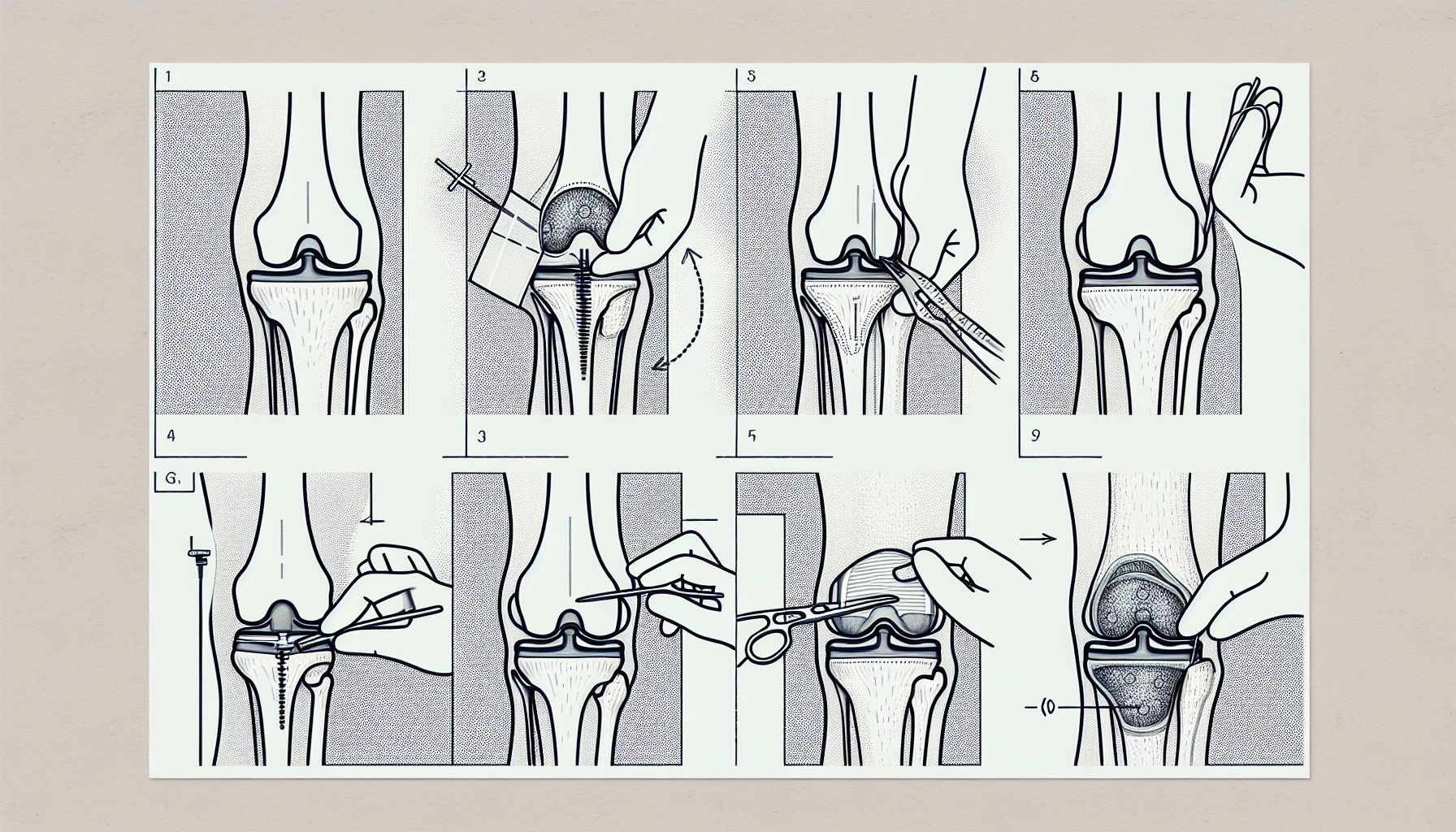
The MIKA surgical procedure is a meticulously orchestrated sequence of precision and skill. It includes the following steps:
- Administration of anesthesia, which can be either general or spinal.
- Crafting a smaller incision to access the knee joint.
- Using specialized instruments to remove damaged cartilage and bone.
- Inserting and aligning the prosthetic components.
- Meticulously closing the incision to foster healing and minimize scarring.
Anesthesia and Incision
The choice of anesthesia is critical for patient comfort and the success of the surgery. General or spinal anesthesia is typically used to ensure that patients remain pain-free during the procedure.
A smaller incision, typically 4 to 6 inches in length, is strategically placed over the middle of the knee to provide optimal access to the joint with minimal tissue disruption.
Implant Alignment and Insertion
The precision of implant alignment and insertion is a testament to the skillful use of specialized instruments tailored for minimally invasive procedures. Surgeons meticulously cut and prepare the damaged portions of the femur and tibia, attach the metal components, and insert a plastic spacer to facilitate smooth knee movement.
Closing the Incision
The final step in the surgical procedure is closing the incision, which is done with great attention to detail to ensure minimal scarring and optimal healing. The joint is cleaned, excess cement is removed, and the skin and muscle layers are surgically closed to complete the procedure.
Postoperative Care and Pain Management

Postoperative care is critical for a successful recovery. Patients are counseled to:
- Apply ice to their knee
- Elevate it above heart level to manage pain and alleviate swelling
- Properly care for their incision and change dressings to prevent infection and promote healing.
Additionally, getting patients moving early has been shown to be safe and beneficial for improving knee function and reducing hospital stay and associated costs.
Managing Pain Post Surgery
Post-surgery pain management is a primary focus for both patients and healthcare providers. Techniques such as continuous femoral nerve block and patient-controlled analgesia (PCA) have proven to be effective in reducing pain, decreasing the need for opioids, and increasing patient satisfaction.
Wound Care Essentials
Proper wound care is vital for preventing infection and encouraging appropriate healing following knee arthroplasty. Here are some key practices to follow:
- Keep the surgical site clean and dry.
- Use sterile dressings to cover the wound.
- Monitor for signs of infection, such as redness, swelling, or discharge.
By following these practices, you can ensure that your wound heals properly and minimize the risk of complications.
Routine follow-ups, including wound checks and progress monitoring, are critical components of postoperative care.
Rehabilitation and Long-Term Recovery
The final stages of the knee replacement journey involve rehabilitation and recovery. Through proper care and following a prescribed exercise regimen, patients often return to activities such as walking, cycling, and swimming within six weeks after surgery.
Long-term outcomes are generally positive, with most implants lasting many years and providing patients with decreased pain and enhanced mobility.
Early Mobilization Strategies
Early mobilization following knee arthroplasty is crucial for enhancing knee motion and expediting recovery. Initiating movement shortly after surgery is safe and can provide benefits such as reduced hospital stay and cost savings.
Prescribed home exercises help strengthen muscles and prevent joint stiffness, contributing to a quicker return to normal activities.
Exercise Regimen and Follow-Up Care
Developing a structured exercise program and attending follow-up appointments are essential for monitoring progress and ensuring a successful recovery. A daily exercise routine, including walking and joint-strengthening exercises, is recommended to promote early recovery and improve joint movement.
Physical therapy may extend for several months post-surgery, supporting safe movement and walking as part of the recovery process.
Innovations in MIKA: Robotic-Assistance and Navigation
Knee arthroplasty, including total knee arthroplasty, is experiencing thrilling innovations like robotic-assisted surgery and computer-assisted navigation, which heighten the precision of surgical procedures, including minimally invasive knee replacements, and improve patient outcomes.
Enhanced recovery protocols are also part of these advancements, aimed at expediting rehabilitation and improving the overall experience for patients.
Robotic-Assisted Surgery
Robotic-assisted surgery represents the cutting edge in the world of MIKA, offering unparalleled precision and tailored surgical planning. Advanced technologies such as the Mako SmartRobotics, CORI Surgical System, and ROSA robotic surgical assistant guide the surgeon’s hand, allowing for more accurate bone cuts and implant positioning. These systems enhance the surgeon’s capabilities with features like 3D CT-based planning, handheld robotics, and X-ray-based 3D imaging, thus promising a future where knee replacements are consistently executed with robotic precision.
Computer-Assisted Navigation
Computer-assisted navigation is another technological marvel that is refining the outcomes of knee arthroplasty. Systems such as OrthoPilot, Vector Vision, and Knee Track Module provide real-time feedback to the surgeon, ensuring that the alignment of the implant is as perfect as possible. While these navigation tools are proving to be valuable in reducing alignment outliers, the long-term impact on the revision rate is still under scrutiny, highlighting the need for ongoing research in this innovative field.
Risks and Complications Associated with MIKA
Like every surgical procedure, MIKA also involves inherent risks. Although minimally invasive techniques aim to reduce the impact of surgery, they are associated with a unique set of challenges and potential complications, such as infection, excessive bleeding, and nerve damage. It is paramount for patients to understand these risks, as severe complications like infections and blood clots occur in a small percentage of cases, necessitating careful consideration and thorough discussions with the surgeon prior to the procedure.
Understanding the Risks
Comprehending the risks tied to MIKA enables patients to make educated decisions regarding their surgery. As surgeons gain more experience with minimally invasive techniques, the rate of complications tends to decrease, yet it’s important to acknowledge that the initial stages of the learning curve do not immediately result in fewer complications.
Techniques such as the quadriceps sparing approach, while beneficial for recovery, may pose challenges in implant alignment, highlighting the need for a highly skilled surgeon to mitigate the risks of revision surgery.
The Role of Patient Selection
Appropriate patient selection significantly impacts the success of MIKA. Various patient-specific factors, such as:
- body weight
- history of knee surgeries play a critical role in determining the appropriateness of minimally invasive techniques for an individual. A comprehensive risk analysis, taking into account:
- age
- gender
- body mass index helps to identify the best candidates for MIKA and minimize the likelihood of complications.
Summary
As we draw the curtain on this exploration of Minimally Invasive Knee Arthroplasty, it’s clear that the world of knee replacement surgery has been transformed by these advanced techniques. MIKA offers a compelling alternative to traditional surgery, with benefits such as smaller incisions, less pain, and rapid recovery times, while also placing a premium on surgeon expertise and patient education. Innovations like robotic-assisted surgery and computer-assisted navigation are pushing the boundaries even further, ensuring that the future of joint replacement is both bright and precise.
Frequently Asked Questions
Is minimally invasive knee replacement surgery right for everyone?
No, minimally invasive knee replacement surgery is not suitable for every patient, as factors such as weight, knee anatomy, and previous surgeries can affect its suitability. A thorough evaluation by an orthopedic surgeon is necessary to determine if it’s the right choice.
What are the key benefits of minimally invasive knee arthroplasty?
Minimally invasive knee arthroplasty offers reduced postoperative pain, faster recovery, smaller scars, and a shorter hospital stay, while achieving outcomes comparable to traditional knee replacement surgery.
How long does it take to recover from minimally invasive knee surgery?
Recovery from minimally invasive knee surgery typically takes around a year, with most patients resuming normal activities about six weeks post-surgery. However, individual recovery timelines may vary based on health, surgical techniques, and rehabilitation effectiveness.
What innovations are currently shaping the future of knee replacement surgery?
Innovations such as robotic-assisted surgery, computer-assisted navigation, and enhanced recovery protocols are currently shaping the future of knee replacement surgery by improving precision and expediting rehabilitation for better patient outcomes.
What are the risks associated with minimally invasive knee replacement surgery?
Minimally invasive knee replacement surgery (MIKA) carries risks such as infection, nerve damage, excessive bleeding, and potential implant misalignment. Patients should thoroughly understand and discuss these risks with their surgeon beforehand to make an informed decision.





 William D. Murrell, MD
William D. Murrell, MD Thomas B. Evely, DO
Thomas B. Evely, DO Clifford Voigt, MD
Clifford Voigt, MD Karthikeyan Chinnakkannu, MD
Karthikeyan Chinnakkannu, MD Max N. Seiter, MD
Max N. Seiter, MD Demetris Delos, MD
Demetris Delos, MD Lauren M. Fabian, MD
Lauren M. Fabian, MD